Understanding Ovarian Cancer: A Guide for Families
Published on April 15, 2024
Updated on April 13, 2024
Published on April 15, 2024
Updated on April 13, 2024
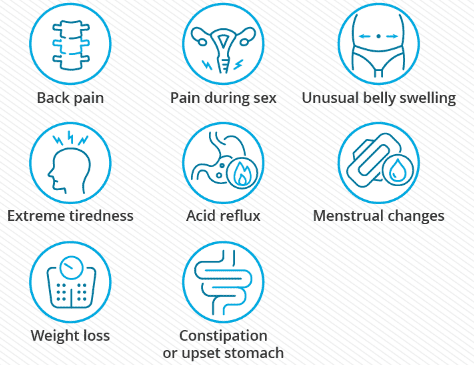
Table of Contents
When a cherished family member receives an ovarian cancer diagnosis, the path ahead can feel daunting and complex. As a hospice registered nurse case manager specializing in empathetic end-of-life care, I am here to offer you clear and compassionate direction. In this article, we will discuss the anticipated stages of ovarian cancer, the transformations you may notice in your loved one, and effective methods to ensure optimal care from diagnosis to the journey's close.
If your loved one has been diagnosed with ovarian cancer, you may have many questions and concerns. Ovarian cancer is a serious disease that affects the female reproductive system. The reproductive system is where babies are made. The ovaries are two small organs that make eggs and hormones. Hormones are chemicals that control how your body works. Sometimes, the cells in the ovaries or nearby areas grow too fast and form a lump called a tumor. This is called ovarian cancer. There are various kinds of ovarian cancer, and some are more common than others. Some things can make your loved one more likely to get ovarian cancer, such as getting older, having a family member who had ovarian cancer, being very overweight, or taking certain medicines after menopause. Menopause is when a woman stops having periods and can no longer have babies. Ovarian cancer can cause some signs that something is wrong, such as feeling full quickly, having pain in the belly or pelvis, having trouble eating, or going to the bathroom more often. But these signs can also be caused by other things, so they are hard to notice. The best way to find out if your loved one has ovarian cancer is to see a doctor who can do some tests and check their health. The doctor can also tell you what kind of treatment your loved one needs. Treatment is what the doctor does to try to make your loved one better. The most common treatments for ovarian cancer are surgery and chemotherapy. Surgery is when the doctor removes the tumor and sometimes other parts of the reproductive system. Chemotherapy is when the doctor gives your loved one special medicine that kill the cancer cells. Ovarian cancer is a scary and challenging thing to deal with, but your loved one is not alone. You can provide them with care and support, such as helping them with daily tasks, listening to their feelings, and encouraging them to follow the doctor's advice. You can also find support for yourself from other people who care for someone with ovarian cancer. They can share their stories and tips with you and make you feel less alone. Ovarian cancer is not your loved one's fault, and they can still have a good and happy life.
Ovarian cancer can be different for different people. One way to describe how much the cancer has grown or spread is to use stages. Stages are numbers that tell you how big the tumor is and where it is in the body. Knowing the stage of the cancer can help you and the doctor decide what kind of treatment is best for your loved one. Here are the main stages of ovarian cancer and what they mean:
This means that the cancer is only in the ovaries or nearby areas, such as the fallopian tubes or the lining of the belly. The fallopian tubes are tubes that connect the ovaries to the uterus, where the baby grows. The lining of the belly is called the peritoneum, and it covers and protects the organs inside. Early stage ovarian cancer is easier to treat than later stages because the cancer has not spread to other parts of the body. The most common treatment for early stage ovarian cancer is surgery, where the doctor removes the tumor and sometimes other parts of the reproductive system. Sometimes, the doctor may also give chemotherapy after surgery to make sure that all the cancer cells are gone. Early stage ovarian cancer may not cause any symptoms, so it can be hard to find. That's why it's important for your loved one to see their doctor regularly and tell them if they notice any changes in their body or how they feel.
This means that the cancer has spread beyond the ovaries and nearby areas to other parts of the belly or even other organs, such as the lungs or the liver. The lungs are where you breathe, and the liver is where you filter your blood. Advanced stage ovarian cancer is harder to treat than early stage ovarian cancer because the cancer has affected more of the body. The most common treatment for advanced stage ovarian cancer is a combination of surgery and chemotherapy. Surgery is where the doctor removes as much of the tumor and the affected organs as possible. Chemotherapy is where the doctor gives your loved one special medicine that kill the cancer cells. Sometimes, the doctor may also use targeted therapies, which are medicines that attack specific features of the cancer cells. Advanced stage ovarian cancer can cause more symptoms, such as swelling or pain in your loved one's belly, changes in their bowel habits, weight loss, or shortness of breath. These symptoms can make your loved one feel uncomfortable or sick, but there are ways to manage them. The doctor can give your loved one medicines or other treatments to help them feel better. You can also help your loved one by doing things like preparing healthy meals, helping them stay active, giving them rest, and comforting them. Advanced stage ovarian cancer can be scary and stressful, but your loved one doesn't have to face it alone. You can show them your love and support, such as being there for them, listening to their worries, and cheering them up. You can also find comfort and hope from other people who have ovarian cancer or who have survived it. They can inspire you and your loved one to keep fighting. Ovarian cancer is not the end of your loved one's story, and they can still enjoy their life and make it meaningful.
Ovarian cancer is a difficult disease, and its journey has different parts. Knowing these parts can help you get ready for what comes next.
Diagnosis and Treatment: When your loved one finds out they have ovarian cancer, their doctors will make a plan to treat it. This may include surgery, chemotherapy, or targeted therapies. Surgery is when the doctors remove the tumor and sometimes other parts of the reproductive system. Chemotherapy is when the doctors give your loved one special medicine that kill the cancer cells. Targeted therapies are medicines that attack specific features of the cancer cells. The treatment plan depends on the type and stage of the cancer, and how your loved one feels. The goal of the treatment is to get rid of the cancer or slow it down.
Symptom Management: Ovarian cancer can cause some signs that something is wrong, such as pain, nausea, and fatigue. Pain is when your loved one feels hurt or sore. Nausea is when your loved one feels sick to their stomach. Fatigue is when your loved one feels very tired. These signs can make your loved one feel bad or sad, but there are ways to help them. As a hospice nurse, I know how to manage these symptoms with medicines or other treatments. Talking to the doctors is especially important to make sure your loved one is comfortable.
End-of-Life Care: As the cancer grows or spreads, hospice care becomes particularly important for making your loved one's life better. Hospice care is when a team of nurses, doctors, and other helpers come to your home or a special place to take care of your loved one. My job is to give your loved one medicines or other treatments to help them feel calm and peaceful. I also give emotional support to your loved one and you. Emotional support is when I listen to your feelings and worries, and help you cope with them. Hospice care is not about giving up, but about making the most of the time you have with your loved one.
Ovarian cancer can cause some changes in your loved one's life. These changes can affect how they look, feel, and act.
Physical Changes: Your loved one may have some changes in their body because of the cancer or the treatment. They may eat less or more, feel more tired or weak, or have trouble moving around. These changes can make your loved one uncomfortable or unhappy, but there are ways to help them. As a hospice nurse, I can give your loved one medicines or other treatments to ease their pain or nausea. I can also help your loved one stay clean and comfortable. You can help your loved one by giving them healthy food and drinks, helping them rest, and keeping them warm.
Emotional Changes: Your loved one may have some changes in their feelings because of the cancer or the treatment. They may feel scared, sad, or unsure about what will happen. These feelings are normal and understandable, but they can also make your loved one feel lonely or hopeless. As a hospice nurse, I can listen to your loved one's feelings and worries and help them cope with them. I can also offer them emotional support and comfort. You can help your loved one by being there for them, talking to them, and cheering them up.
Practical Changes: Your loved one may have some changes in their daily life because of the cancer or the treatment. They may need more help with things like dressing, bathing, or cooking. They may also need more medical equipment or supplies at home. These changes can make your loved one feel dependent or frustrated, but they can also make your life easier and safer. As a hospice nurse, I can teach you how to care for your loved one at home and provide you with the necessary equipment and supplies. I can also help you coordinate with other helpers, such as doctors, social workers, or volunteers. You can help your loved one by learning how to care for them, following the doctor's instructions, and asking for help when you need it.
When your loved one has ovarian cancer, you want to give them the best care possible. You want to show them that you love them and understand what they are going through. You also want to take care of yourself and your own needs. Caring for a loved one with ovarian cancer takes empathy and practical strategies. Here are some topics that can help you provide compassionate care:
Open Communication: Talking honestly with your loved one about their cancer, their treatment, and their wishes is especially important. It can help you and your loved one make decisions together, plan for the future, and cope with the emotions. But talking about these things can also be hard and scary. You may not know what to say, how to say it, or when to say it. You may worry about hurting your loved one's feelings or making them lose hope. My articles provide guidance on how to have these conversations. They give you tips on how to start the conversation, what questions to ask, what words to use, and how to listen. They also help you respect your loved one's choices, even if they are different from yours.
Comfort and Pain Management: Making your loved one comfortable is one of your main goals. You want to ease their pain and make them feel better. But sometimes, pain can be hard to control or manage. It can affect your loved one's mood, sleep, and quality of life. As a hospice nurse, I specialize in providing medications and techniques that relieve pain and promote comfort. My articles explain how pain works, how to measure it, and how to treat it. They also give you advice on how to use medicines safely and effectively, and how to prevent or manage side effects. They also suggest other ways to make your loved one comfortable, such as massage, music, or aromatherapy.
Emotional Support: Ovarian cancer can affect your loved one's emotional health too. They may feel anxious, sad, or uncertain about what will happen. They may also feel angry, guilty, or lonely. These feelings are normal and understandable, but they can also make your loved one feel worse. As a hospice nurse, I understand the emotional toll of ovarian cancer. My articles offer insights into supporting your loved one emotionally. They help you recognize and validate your loved one's feelings and offer them comfort and encouragement. They also help you support yourself emotionally, by giving you tips on how to cope with stress, grief, and burnout. They also remind you to seek help from others, such as friends, family, or counselors.
Creating Meaningful Moments: Spending time with your loved one is precious. You want to make the most of the time you have together and create memories that you can cherish. You also want to help your loved one find meaning and purpose in their life and celebrate their achievements and legacy. My articles provide ideas for creating meaningful moments with your loved one. They suggest activities that you can do together, such as reading, watching movies, or playing games. They also help you create special occasions, such as birthdays, anniversaries, or holidays. They also help you document your loved one's life story, such as writing a letter, making a scrapbook, or recording a video. They also help you say goodbye, such as expressing your love, gratitude, and forgiveness.
There may come a time when the cancer treatment is no longer working, and your loved one is nearing the end of life. This can be an exceedingly difficult and emotional time for both of you. You may feel sad, angry, scared, or numb. You may also have many questions and concerns about what will happen and how to help your loved one. This section will give tips on providing end-of-life care and ensuring comfort and peace for your loved one.
Hospice Care: Hospice care focuses on making your loved one as comfortable as possible in the last months, weeks, or days of life. Hospice care does not try to cure cancer or prolong life but rather to relieve pain and other symptoms, such as nausea, shortness of breath, or anxiety. Hospice care also provides emotional and spiritual support for your loved one and family. Hospice care can be given at home, in a hospital, or at a hospice facility, depending on your loved one's needs and preferences. You can help your loved one by:
Emotional Well-being: The end of life can be a time of mixed emotions for your loved one and family. Your loved one may feel grateful, peaceful, or relieved but also sad, angry, or scared. They may also have regrets, unfinished business, or unfulfilled dreams. You can help your loved one by:
Ovarian cancer is a hard disease, but you and your loved one can face it with courage and love. You can give your loved one the best care possible by being empathic, understanding, and informed. You can also take care of yourself and your own needs by getting support from others. You are not alone on this journey, and there are many people and resources that can help you and your loved one. You can find more information and support from these sources:
Caring for a Loved One with Terminal Cancer: A Guide for Families
Understanding Cancer Metastasis: A Guide for Patients and Families
Ovarian Cancer: Symptoms, Diagnosis & Treatment
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What's the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
Medicare — Find and compare hospice providers
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Cancer Caregiving A-to-Z: An At-Home Guide for Patients and Families
Things I Wish I'd Known: Cancer Caregivers Speak Out
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver's Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I've Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death