Tag: Shortness of Breath
Articles about managing shortness of breath, dyspnea, in the terminally ill.
Articles about managing shortness of breath, dyspnea, in the terminally ill.

This article provides practical tips and strategies for caregivers and family members to prevent dementia patients from removing their oxygen nasal cannula. Ensuring continuous oxygen use is essential for their health and well-being.

Explore the role of oxygen saturation in hospice care, where comfort takes precedence over numbers. Learn how hospice teams prioritize quality of life, interpret vital signs differently, and make ethical decisions about oxygen use. Discover a compassionate approach focused on dignity and peace.

Discover effective strategies for managing end-of-life crises in hospice care. Learn how to recognize signs of distress, implement calming techniques, and provide compassionate support to patients and families. This guide offers practical tips for hospice nurses and caregivers to navigate challenging situations with confidence and empathy.

Caregivers can find it challenging to ensure dementia patients wear their CPAPs overnight. This article offers practical tips and strategies to help caregivers ensure comfortable and uninterrupted CPAP use for their loved ones.

Discover effective non-pharmacological methods to manage shortness of breath in hospice care. Learn about positioning techniques, breathing exercises, and environmental adjustments that can comfort and relieve patients experiencing dyspnea, enhancing their quality of life during end-of-life care.
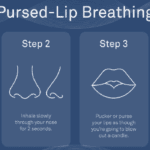
Dealing with shortness of breath can be challenging for terminally ill patients, but there are techniques that can help manage this symptom and improve their overall comfort. One such technique is pursed lip breathing. Pursed lip breathing is a simple and effective breathing technique that can help reduce shortness of breath and improve oxygen exchange in the lungs. As an experienced hospice nurse with years of experience, I will guide you through the steps of pursed lip breathing in a compassionate and easy-to-understand manner.

I have cared for many terminally ill patients over the years. One question that comes up frequently is should the dying patient be on oxygen at the end of life?
I see it from both sides, from hospice intake personnel as well as the admitting nurse — all had it drilled into them over the years that low oxygen saturation must be treated — to families who see how hospital and nursing home staff rush to put someone on oxygen because of low oxygen saturation.
Contrary to widespread belief, most dying patients do not need oxygen. Here’s why:

Guide to Recognize and Treat Common End of Life Symptoms provides tips on managing symptoms experienced by those at the end of their lives - Topics such as pain, shortness of breath, respiratory distress, and anxiety, and provides suggestions for medications and complementary therapies to help manage these symptoms.
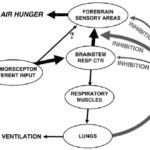
I can count the times I’ve run into air hunger at the end of life as a visiting RN Case Manager for going on five years on one hand. Over the years, I’ve managed patients with pulmonary fibrosis, lung cancers (diverse types), breast cancer, COPD, congestive heart failure, B-cell lymphoma, leukemia, and other diseases that can impact one person’s ability to breathe correctly. Air hunger is rare in my firsthand experiences, but it can happen.
Air hunger often sounds like the person is gasping for breath without regard to the actual respiratory rate (how fast they are breathing); it can also sound like stridor (YouTube videos below where you can hear the difference).