Understanding Hospice Eval and Treat Orders
Published on April 3, 2024
Updated on October 29, 2024
Published on April 3, 2024
Updated on October 29, 2024
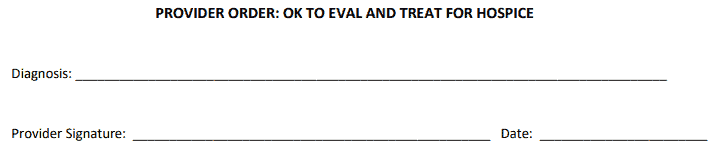
Table of Contents
In healthcare, when a provider writes an order to “Eval and Treat” for hospice, they ask for a thorough evaluation and a tailored treatment plan. This is specifically meant for patients who are being considered for hospice care. Let’s delve into what this means and why it’s crucial.
When someone is extremely sick and needs special care, they might go to hospice. Hospice is not a hospital but a home-like setting where people can be comfortable and peaceful. Hospice helps people who have a serious illness that cannot be cured, such as cancer, heart disease, or Alzheimer’s. Hospice also helps their families and loved ones cope with the situation.
Sometimes, a doctor or a nurse might write an order to “Eval and Treat” for hospice. This means that they want two important things to happen:
Evaluating: This means a team of hospice professionals will visit the person and check their progress. They will ask questions, perform tests, and observe the person’s body and mind. They will also talk to the person and their family about their wishes, needs, and goals and try to understand the person’s situation as best as possible.
Treating: After evaluating the person, the hospice team will make a plan to take care of them. Depending on their condition, symptoms, and preferences, this plan will differ for each person. The plan will include medicine, equipment, therapy, counseling, and other services. The plan will aim to make the person feel as comfortable, pain-free, and happy as possible. The plan will also emotionally, spiritually, and practically support the person’s family and loved ones.
The order to “Eval and Treat” for hospice is a way of saying that the person deserves the best care possible, no matter what. It is a way of showing respect, compassion, and kindness to the person and their family. Hospice is not about giving up hope but about finding hope differently. Hospice is about living well, even when facing death.
When and Why: Sometimes, people get extremely sick, and the doctors say they cannot improve them. This can be extremely hard to accept, but it does not mean they must suffer or be alone. A special kind of care called hospice care can help them and their families.
Hospice care is for people who have a serious illness that cannot be cured and have decided to stop trying treatments that might harm them more than help them. Hospice care is not about dying but about living as well as possible until the end of life. Hospice care is about making someone feel comfortable, peaceful, and loved.
Hospice care is provided by a team of professionals who care for extremely sick people. The team includes doctors, nurses, social workers, counselors, chaplains, volunteers, and others. They work together to provide physical, emotional, spiritual, and practical support to the person and their family. They also respect the person’s wishes, beliefs, and values.
Hospice care can be given in various places, depending on the person’s needs and preferences. Some people choose to receive hospice care at home, where their loved ones and familiar things can surround them. Some people choose to receive hospice care in a hospice facility, where they can get more medical attention and comfort. Some people receive hospice care in a hospital, nursing home, or assisted living facility, where they can be close to other services and staff.
Hospice care is a special kind that can significantly improve the lives of extremely sick people and their families. It can help them cope with the challenges and changes of a serious illness and find hope, meaning, and joy in their final days. Hospice care is a gift of compassion and dignity that everyone deserves.
Purpose: The order to “Eval and Treat” for hospice is especially important because it helps to decide if the person can get hospice care. Hospice care is only for people who have a serious illness that cannot be cured and have a limited time to live. The order means that the person’s health and situation need to be checked carefully to see if they qualify for hospice care.
Comprehensive Assessment: To do this, a team of healthcare experts might visit the person and their family. The team can include doctors, nurses, social workers, and others who know how to care for people who are extremely sick. They will work together to evaluate the person’s condition, symptoms, needs, and goals. They will also ask the person and their family about their wishes, feelings, and concerns. However, the person who oversees the evaluation and admission process is usually a registered nurse. A registered nurse is a nurse with special training and skills to take care of people who are extremely sick. The registered nurse will make sure that the person meets the criteria for hospice care and will explain the benefits and services that hospice care can offer. The registered nurse will also answer any questions the person and their family might have. The registered nurse will be the main contact person for the person and their family throughout the hospice care journey.
Comfort is Key: The treatment plan is the most important part of hospice care. It is made just for the person and their family. It is based on the hospice team’s evaluation and the person’s wishes and needs. The treatment plan focuses on ensuring the person is comfortable and well. Comfort means different things for different people, but it usually means feeling less pain, less stress, and more peace.
Elements of the Plan: The treatment plan might include different things to help the person feel better. Some of these things are:
The treatment plan is a way of showing care and respect to the person and their family. It is a way of helping them live well and die well. The treatment plan is not fixed but flexible. It can change as the person’s condition and needs change. The hospice team will always communicate with the person and their family about the treatment plan and ensure they are satisfied. The hospice team will always support the person and their family throughout the hospice care journey.
Judgement Skills: The admitting party is the person who decides if the person can get hospice care. They are often a registered nurse, but they can also be a doctor or a nurse practitioner. They have a lot of experience and knowledge in caring for people who are extremely sick. They must use their clinical judgment to ask critical questions. Critical questions help them better understand the person’s health and situation. Some examples of critical questions are:
The admitting party must listen carefully to the answers and observe the person’s condition. They must also check the person’s medical records and talk to other healthcare providers who know the person. They must use all this information to make a good decision.
Evaluating Eligibility: Remember, the first step is evaluating if the person is eligible for hospice care. Eligible means that the person meets the criteria for hospice care. The criteria for hospice care are:
If the person meets these criteria, the admitting party can say they are eligible for hospice care. If the person does not meet these criteria, the admitting party can say they are not eligible for hospice care. The admitting party must explain their decision to the person and their family and respect the person’s right to accept or decline hospice care.
If the person is eligible and agrees to hospice care, then comes the admission part. The admission part is when the person officially becomes a hospice patient. The admitting party will help the person and their family fill out some forms and sign some papers. They will also explain what to expect from hospice care and answer any questions that they might have. They will also introduce the person and their family to the hospice team and start the treatment plan. The admitting party will stay in touch with the person and their family throughout the hospice care journey. They will also coordinate with the hospice team and other healthcare providers to ensure that the person receives the best care possible.
Why Hospice? Why Now?: The nurse should start by understanding why the person, family, and caregivers have chosen hospice care. Hospice care is a big decision that can be hard to make. The nurse should ask the person and their family about their reasons and feelings for choosing hospice care. The nurse should also ask them about their expectations and hopes for hospice care. The nurse should listen with empathy and respect. The nurse should also explain the benefits and services that hospice care can provide. The nurse should ensure that the person and their family understand what hospice care is and is not. The nurse should also ensure that the person and their family are comfortable and ready for hospice care.
Painting the Picture: After understanding why the person and their family have chosen hospice care, the nurse should ask critical questions to build a clear picture of the person’s terminal condition. A terminal condition means that the person has a serious illness that cannot be cured and will probably cause their death soon. The nurse should ask the person and their family about their medical history, current symptoms, medications, treatments, and other health issues. The nurse should also do a physical examination and check the person’s vital signs, such as blood pressure, heart rate, and temperature. The nurse should also observe the person’s appearance, behavior, and mood. The nurse should use all this information to assess the person’s health and well-being. The nurse’s assessment should align with key guidelines.
Key guidelines help the nurse decide if the person is eligible for hospice care. The key guidelines are based on the person’s diagnosis, prognosis, and functional status. Diagnosis means the name of the illness that the person has. Prognosis means the expected outcome of the illness. Functional status means the ability of the person to do daily activities, such as eating, dressing, bathing, and walking. The key guidelines vary depending on the type of illness that the person has, but they generally require that the person has a life expectancy of six months or less if the illness follows its normal course. The nurse should compare the person’s condition to the key guidelines and determine if the person meets the criteria for hospice care. The nurse should also document the person’s condition and the key guidelines in the person’s medical record.
Hospice care is a special kind of care that helps people who are extremely sick and their families. To get hospice care, a person needs an order to “Eval and Treat” for hospice. This order means that a nurse or another healthcare expert will visit the person and their family to check if they can get hospice care. The nurse will ask many questions and do some tests to understand the person’s health and situation. The nurse will also make a plan to take care of the person and their family. The plan will include things that will make the person feel comfortable, happy, and loved. The nurse will also explain everything to the person and their family and answer any questions.
The order to “Eval and Treat” for hospice is especially important because it helps the person and their family get the best care possible. The nurse’s role is to ensure that the person is eligible for hospice care and help them start their hospice care journey. The nurse’s role is to be kind, respectful, and supportive to the person and their family. The nurse’s role is to make a difference in the person’s and their family’s life.
Understanding Hospice Care: Is it Too Early to Start Hospice?
Picking a hospice agency to provide hospice services
What’s the process of getting your loved one on hospice service?
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying