Understanding Mild Cognitive Impairment: A Guide for Patients and Families
Published on May 1, 2024
Updated on August 1, 2025
Published on May 1, 2024
Updated on August 1, 2025
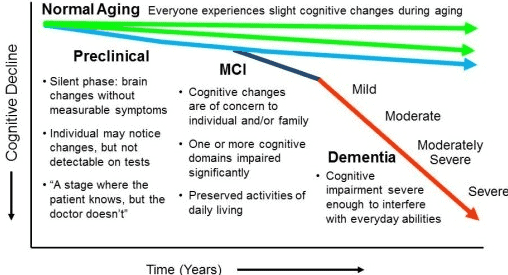
Table of Contents
It can be worrying when someone we love starts forgetting little things, like where they left their keys or the name of a neighbor they’ve known for years. It’s important to understand that these moments can be signs of Mild Cognitive Impairment, or MCI for short.
MCI is like a middle ground between the expected memory loss of normal aging and the more severe decline of dementia. People with MCI have more memory problems than expected for their age, but they can still take care of themselves and do their daily activities. It’s not as severe as dementia, where these memory and thinking problems are big enough to interfere with someone’s daily life.
Finding out about MCI early is significant. It’s like spotting a small leak in your house before it causes much damage. If we catch these changes early, we can do something about it. We can look for ways to help our loved ones keep their memory and thinking skills and maybe even improve them. Plus, knowing about MCI early gives families time to plan for the future, talk about care options, and make decisions together.
Remember, having MCI doesn’t mean someone will get dementia, but it does mean we should pay attention and take steps to help our loved ones stay as sharp as they can for as long as possible. It’s all about caring for each other and facing these challenges with hope and support.
It’s not always easy to tell if a loved one is experiencing a bit of forgetfulness that comes with getting older or if it’s something more. Knowing the signs of Mild Cognitive Impairment (MCI) can help.
MCI can show up in different ways. Some common signs include:
These symptoms are more than just the occasional memory slip; they’re not so severe that they stop someone from living normally.
If you notice these signs in your loved one, it might be time to talk to a doctor. It’s like when a warning light comes on in your car; it doesn’t mean the car is about to break down, but it’s a good idea to get it checked out. The same goes for memory changes.
Seeing a doctor can help determine whether these signs are MCI or something else. Plus, it can give you peace of mind and a plan for what to do next. It’s all about taking that first step to care for your loved one’s health, just like you would for any other important part of their life. Remember, you’re not alone in this. A whole community of families and caregivers is out there who understand and can offer support.
When we start to notice changes in our loved one’s memory or thinking, it’s natural to feel a mix of concern and hope. That’s when medical professionals step in to help us understand what’s happening.
Doctors and healthcare teams are like detectives for health. They look at all the clues – the symptoms we’ve noticed – and use their knowledge to discover what’s causing them. For MCI, they’ll talk to us and our loved ones, ask about the changes we’ve seen, and learn about our family’s health history. They’re there to listen, understand, and guide us through the following steps.
Doctors will do a few tests to determine if someone has MCI. These might include:
Sometimes, doctors might also suggest brain scans or blood tests to rule out other causes of the symptoms. This is done gently and carefully, ensuring our loved ones feel safe and respected.
The goal of these tests isn’t just to put a name to what’s happening but to help us find the best way to support our loved ones. Whether it’s finding activities to keep their minds active or connecting with local support groups, the tests give us a starting point. And throughout this journey, we’re not alone. The medical team is with us, offering their expertise and compassion every step of the way.
Learning that a loved one has Mild Cognitive Impairment (MCI) can bring a lot of questions and worries about the future, especially when it comes to dementia. Let’s talk about what this means and what we can expect.
Think of MCI as a signal. It’s like a light on your car’s dashboard that tells you something needs attention. MCI is a sign that changes are happening in the brain. These changes might be small and stay that way, or they could be the start of a more significant journey towards dementia.
Dementia is a group of symptoms that affect memory, thinking, and social abilities enough to interfere with daily life. It’s not a specific disease, but several diseases can cause dementia, like Alzheimer’s disease. MCI can be one of the first signs that these diseases are developing.
Here’s the hopeful part: having MCI doesn’t mean dementia is inevitable. It’s like being at a crossroads rather than on a one-way street. Some people with MCI stay the same for years, some even get better, and yes, some do progress to dementia. But it’s not a guarantee.
What’s important is that we use this time to do everything we can to support our loved ones. There are ways to help keep their minds active and engaged, which might slow any progression. This includes things like puzzles, social activities, and maybe even changes in diet and exercise.
It’s also a time to cherish the moments we have with our loved ones. Every day is a gift, and MCI reminds us to make the most of our time together. We can’t predict the future but can fill our days with love, support, and care. And no matter what happens, we’ll face it as a family with strength and hope.
Adjusting to life with Mild Cognitive Impairment (MCI) can be like learning a new dance. It takes patience, practice, and support, but with time, it can become a rhythm you and your loved one can manage together.
Living with MCI means making minor changes to help your loved one stay independent and engaged. Here are some ideas:
You’re not dancing this dance alone. Many people and places can help:
Remember, every family’s dance with MCI is unique. It’s about finding the steps that work best for you and your loved one, and sometimes, it’s about taking a moment to enjoy the music, even amidst the challenges.
Navigating life with Mild Cognitive Impairment (MCI) can be a journey filled with love, patience, and understanding. Here are some strategies to help make this journey smoother for patients and caregivers.
Keeping the brain active is like giving it a daily workout. Here are some exercises that can help:
Just like we care for our bodies, we must care for our brains. Here are some lifestyle changes that can help:
Remember, these strategies are not just tasks to check off; they’re opportunities to spend quality time with your loved one and create joyful moments together. It’s about building a supportive environment where patients and caregivers can thrive.
When a family member has Mild Cognitive Impairment (MCI), planning for the future becomes an act of love and foresight. It’s about making sure that, no matter what happens, your loved one’s wishes are respected and their needs are met.
It’s essential to think about legal and financial matters early on. Here’s what you can do:
As MCI progresses, you might need to consider long-term care options. These can include:
Hospice care is about providing comfort and dignity near the end of life. It’s not just for the final days; it can be helpful for anyone with a life expectancy of six months or less. If your loved one’s health declines significantly, hospice can offer support for both the patient and the family.
Remember, planning doesn’t mean giving up hope. It’s about being prepared and finding peace of mind in knowing you’re doing everything possible to care for your loved one.
As we end our journey through understanding Mild Cognitive Impairment (MCI), we must recognize that knowledge is a powerful tool. It can light the way through uncertain times and strengthen us to make the best decisions for our loved ones.
Learning about MCI has given us the power to take action and to feel more in control of the situation. We’ve learned about the signs to watch for, the importance of early detection, and the steps to support our loved ones. With this knowledge, we can create a nurturing environment that encourages our family members to maintain their independence and quality of life for as long as possible.
The path forward with MCI is one of hope and proactive care. It’s about taking each day as it comes, enjoying the good moments, and facing the challenges with courage. We can’t predict the future, but we can walk this path with our heads held high, knowing we’re doing everything possible to support and protect those we love.
Remember, you’re not alone on this journey. A community of caregivers and families is walking a similar path, ready to offer support and understanding. We can face the future with hope and a shared commitment to caring for our loved ones.
Mild Cognitive Impairment (MCI)
Mild Cognitive Impairment: It’s Not ‘Normal’ Aging
Staving off dementia when you have mild cognitive impairment
Eye-tracking paradigms for the assessment of mild cognitive impairment: a systematic review
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Dementia Home Care: How to Prepare Before, During, and After
DEMENTIA DENIED: One Woman’s True Story of Surviving a Terminal Diagnosis & Reclaiming Her Life
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
Fading Reflection: Understanding the complexities of Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy. (Video)
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
How Do I Know You? Dementia at the End of Life
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?