Understanding Bacteremia and Sepsis in the Geriatric Population: A Comprehensive Guide
Published on June 18, 2025
Updated on June 18, 2025
Published on June 18, 2025
Updated on June 18, 2025
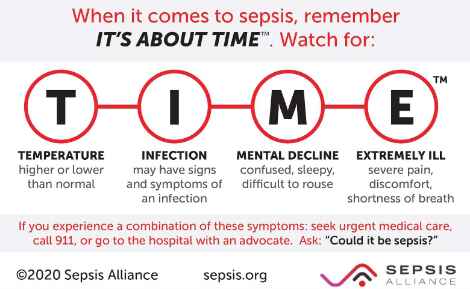
Table of Contents
As a caregiver or family member of an elderly loved one, you play a crucial role in their health and well-being. Today, we will discuss two severe conditions that can affect older adults: bacteremia and sepsis. While these terms may sound intimidating, understanding them can help you protect your loved one and recognize when they require medical attention.
Let’s break down these terms:
Here’s a simple table to help you understand the relationship between these conditions:
| Condition | Description | Can it lead to Sepsis? |
|---|---|---|
| Bacteremia | Bacteria in the blood | Yes, if left untreated |
| Sepsis | Severe body response to infection | Already a serious condition |
It’s essential to note that not all cases of bacteremia result in sepsis; however, it’s a medical emergency when they do.
You might wonder, “Why are we focusing on older adults?” Here’s why:
The good news is that with your help, many cases can be prevented or caught early.
Here are some key points to remember:
Your role as a caregiver or family member is invaluable. By learning about these conditions, you’re taking an essential step in protecting your loved one’s health. In the following sections, we’ll explore how to recognize signs of trouble, prevent infections, and know when to get help.
Remember, you’re not alone in this journey. Healthcare providers, including hospice nurses like me, are here to support you and your loved one every step of the way. Together, we can work to keep your elderly family member as healthy and comfortable as possible.
As a caregiver or family member, it’s essential to understand these conditions to support your loved one better. Let’s break down the key concepts:
Bacteremia and sepsis are related but distinct conditions:
Here’s a table to help you understand the key differences:
| Condition | Definition | Symptoms | Severity |
|---|---|---|---|
| Bacteremia | Bacteria in the blood | Often, no symptoms; may clear on their own | It can be mild to severe |
| Sepsis | The body’s extreme response to infection | Fever, rapid breathing, confusion, etc. | Always serious, it can be life-threatening |
Important: Bacteremia can lead to sepsis if left untreated, but not all cases of bacteremia progress to sepsis.
Understanding how these conditions develop in the body can help you grasp their seriousness:
Bacteremia:
Sepsis:
Both bacteremia and sepsis can stem from various sources. Here are some common causes:
Risk factors that make someone more susceptible include:
Remember: As a caregiver, you play a crucial role in prevention and early detection. Watch for signs of infection and seek medical help promptly if you’re concerned.
Understanding these conditions will better equip you to support your loved one and communicate effectively with healthcare providers. Always consult with medical professionals for personalized advice and care.
Caring for an elderly loved one involves understanding the unique risks they face, especially when it comes to severe conditions like bacteremia and sepsis. Let’s examine the key risk factors that increase the susceptibility of older adults to these infections.
As we age, our bodies undergo several changes that can increase the risk of infections:
Key Points to Remember:
Many elderly individuals have multiple chronic health conditions, known as comorbidities, which can complicate their health:
Important Note: Effectively managing these conditions can help reduce the risk of infections. Regular check-ups and following prescribed treatments are crucial.
Living in a long-term care facility or frequent hospital visits can increase the risk of infections:
Preventive Measures:
Medical devices are often necessary, but can also pose risks:
Tips for Caregivers:
| Risk Factor | Description | Prevention Tips |
|---|---|---|
| Age-Related Changes | Weakened immune system, thinner skin, reduced organ function | Look for atypical signs of infection, and maintain good hygiene |
| Comorbidities | Multiple chronic conditions like diabetes, heart disease, and COPD | Manage conditions effectively, and regular check-ups |
| Institutionalization and Hospitalization | Close contact, exposure to resistant bacteria, and frequent procedures | Ensure proper hygiene, limit invasive devices |
| Use of Medical Devices | Urinary catheters, IV lines, ventilators | Monitor closely, follow cleaning protocols, and report infection signs |
Understanding these risk factors can help protect your elderly loved one from severe infections, such as bacteremia and sepsis. Always consult with healthcare providers for personalized advice and support. Your vigilance and care can have a significant impact on their health and well-being.
Preventing infections that can lead to bacteremia and sepsis is crucial, especially for older adults. Here are some effective strategies to help keep your loved ones safe.
Good hygiene practices are the first line of defense against infections. Here are some key steps:
Hand Hygiene:
Wound Care:
Personal Hygiene:
Environmental Hygiene:
Catheters are often necessary, but can increase the risk of infection if not managed properly. Here are some tips:
Urinary Catheters:
Intravenous (IV) Lines:
Antibiotic stewardship involves using antibiotics responsibly to prevent the development of resistance and ensure their continued effectiveness. Here are some guidelines:
Use Antibiotics Only When Necessary:
Complete the Full Course:
Avoid Misuse:
| Prevention Strategy | Key Actions |
|---|---|
| General Hygiene | Wash hands, clean wounds, and maintain personal and environmental hygiene |
| Catheter Management | Use only when necessary, complete the entire course, and avoid misuse |
| Antibiotic Stewardship | Use only when necessary, complete the full course, and avoid misuse |
Following these prevention strategies can significantly reduce the risk of infections leading to bacteremia and sepsis in your elderly loved ones. Always consult with healthcare providers for personalized advice and support. Your proactive care and attention can have a significant impact on their health and well-being.
Early detection of bacteremia and sepsis is crucial for improving outcomes, especially in the elderly. Recognizing symptoms early and understanding the diagnostic tools available can make a significant difference.
Older adults may not always exhibit the typical symptoms of infections or sepsis. Here’s what to look for:
In the elderly, symptoms of bacteremia and sepsis can be subtle or atypical. This means they might not exhibit the usual signs, such as fever. Instead, you might notice:
Important Note: These atypical symptoms can delay diagnosis, so being vigilant and proactive is essential.
While symptoms can vary, some common signs of sepsis in the elderly include:
Remember: If you notice any of these symptoms, especially when they occur together, seek medical help immediately.
Diagnosing sepsis involves a combination of physical examinations, medical history, and various diagnostic tests. Here are some common diagnostic tools:
| Test | Purpose | What It Shows |
|---|---|---|
| Complete Blood Count (CBC) | Measures white blood cells | A high or low WBC count can indicate infection |
| Blood Cultures | Identifies bacteria in the blood | Helps determine the type of bacteria causing the infection |
| Lactate Levels | Measures lactic acid | High levels can indicate poor oxygen delivery to tissues |
| C-reactive protein (CRP) | Measures inflammation | High levels suggest inflammation, possibly due to infection |
| Prothrombin Time (PT) and Partial Thromboplastin Time (PTT) | Measures blood clotting | Abnormal results can indicate sepsis-related clotting issues |
Additional Tests:
Timely diagnosis of sepsis is critical for several reasons:
Key Points to Remember:
By understanding these early detection strategies and being vigilant about changes in your loved one’s health, you can help ensure they receive the timely care they need. Always consult with healthcare providers for personalized advice and support. Your attentiveness and care can have a significant impact on their health and well-being.
Timely and effective management is crucial when treating bacteremia and sepsis in the elderly. Here, we’ll cover the main treatment strategies, including initial management, antibiotic therapy, and supportive care.
Initial management focuses on stabilizing the patient and addressing the immediate threats posed by sepsis. Here are the key steps:
Fluid resuscitation is one of the first steps in treating sepsis. It helps maintain blood pressure and ensures that organs receive enough blood and oxygen.
Important Note: Fluid resuscitation is crucial in the early stages to prevent organ failure.
If fluid resuscitation does not adequately raise blood pressure, vasopressors may be needed.
Key Point: Vasopressors are used when blood pressure remains low despite adequate fluid resuscitation.
Antibiotics are essential for treating the infection causing sepsis. Here’s how they are managed:
Common Antibiotics:
Important Note: Completing the full course of antibiotics is crucial to ensure the infection is fully eradicated.
Supportive care focuses on the patient’s overall well-being, helping to manage symptoms and complications.
Proper nutrition is vital for recovery. Here’s how to support your loved one’s nutritional needs:
Key Point: Adequate nutrition supports the immune system and aids in recovery.
Managing existing health conditions is crucial for improving outcomes and preventing complications.
Important Note: Regular communication with healthcare providers is crucial for effectively managing these conditions.
| Treatment Approach | Key Actions |
|---|---|
| Fluid Resuscitation | Administer 30 mL/kg IV fluids within the first hour, monitor vital signs |
| Use of Vasopressors | If blood pressure remains low after fluids, a common choice is norepinephrine. |
| Antibiotic Therapy | Start with broad-spectrum antibiotics and narrow down based on culture results; the typical duration is about two weeks. |
| Nutritional Support | Assess nutritional needs and provide enteral or parenteral nutrition if needed. |
| Management of Comorbid Conditions | Monitor and adjust treatments for diabetes, heart disease, COPD |
By understanding these treatment approaches, you can better support your elderly loved one through their recovery from bacteremia and sepsis. Always consult with healthcare providers for personalized advice and support. Your attentiveness and care can have a significant impact on their health and well-being.
Caring for an elderly loved one with bacteremia or sepsis can be a daunting experience. Understanding the challenges can help you provide more effective support and work more efficiently with healthcare providers. Let’s explore some fundamental difficulties in managing these conditions in older adults.
Identifying bacteremia and sepsis in older adults can be tricky for several reasons:
Atypical symptoms: Older adults may not show the usual signs of infection, such as fever. Instead, you might notice:
Overlapping symptoms: Many symptoms of infection can be similar to those of other conditions common in the elderly, making diagnosis more difficult.
Communication barriers: Some older adults may have difficulty describing their symptoms due to cognitive impairments or communication difficulties.
Important note: Trust your instincts. Don’t hesitate to seek medical attention if you notice any sudden changes in your loved one’s behavior or health.
Once diagnosed, treating bacteremia and sepsis in older adults can present its own set of challenges:
Key point: Always provide healthcare providers with a complete list of your loved one’s medications and health conditions to help avoid complications.
Caring for an elderly person with a severe infection like sepsis can involve some difficult decisions:
Remember: These decisions are never easy, but open communication with healthcare providers and family members can help guide you.
| Challenge Type | Key Points |
|---|---|
| Diagnostic Challenges | – Atypical symptoms – Overlapping symptoms with other conditions – Communication barriers |
| Treatment Complications | – Multiple medication interactions – Altered drug metabolism – Weakened immune system – Impact of underlying health conditions |
| Ethical Considerations | – Decisions on treatment intensity – Balancing quality of life with aggressive treatment – End-of-life care discussions – Respecting patient autonomy |
Navigating these challenges can be overwhelming, but remember, you’re not alone. Healthcare providers support you and your loved one through this difficult time. Don’t hesitate to ask questions, seek clarification, or express your concerns. Your attentiveness and care can have a significant impact on your loved one’s health and well-being.
As a caregiver or family member of an elderly loved one who has experienced bacteremia or sepsis, it’s essential to understand that recovery can be a long journey. Let’s explore the long-term outcomes and what you can expect during the follow-up period.
Bacteremia and sepsis can have severe consequences for older adults:
Important note: While these statistics may seem alarming, many older adults survive and recover. Each person’s situation is unique.
Surviving sepsis doesn’t mean the journey is over. Many older adults experience ongoing challenges:
Physical function: Weakness and fatigue are common, affecting daily activities.
Cognitive function: Memory, attention, and problem-solving skills may be impacted. Sepsis can accelerate long-term cognitive decline by about 0.02 points per year on cognitive tests.
Emotional health: Depression, anxiety, and post-traumatic stress disorder (PTSD) are not uncommon.
Key point: These changes can be gradual and may not be immediately apparent after discharge from the hospital.
Recovery is possible, but it often requires patience and support:
Recovery timeline: The process can take anywhere from months to years. It’s essential to set realistic expectations and celebrate small victories.
Regular follow-up is crucial for monitoring recovery and addressing any new issues:
| Follow-Up Aspect | Frequency | Purpose |
|---|---|---|
| Primary Care Visits | Every 1-3 months initially | Monitor overall health, adjust medications |
| Specialist Visits | As needed | Address specific organ system issues |
| Cognitive Assessments | Every 6-12 months | Track cognitive function over time |
| Physical Therapy | Weekly or bi-weekly | Improve strength and mobility |
| Mental Health Check-ins | Monthly or as needed | Address emotional well-being |
Remember: As a caregiver, you play a vital role in this follow-up process. Keep track of appointments, medications, and any new symptoms or concerns.
By understanding these long-term outcomes and actively participating in the follow-up process, you can provide the best support for your loved one’s recovery journey. Remember, healthcare providers are there to guide you through this process, so don’t hesitate to ask questions or seek additional support when needed.
Caring for an elderly loved one with bacteremia or sepsis can be challenging and emotionally taxing. Understanding these conditions, their risk factors, prevention strategies, early detection, treatment approaches, and long-term outcomes is crucial for providing the best care possible. Let’s summarize the key points, examine future directions and research needs, and highlight some valuable resources for patients and caregivers.
Here’s a quick recap of the essential information covered:
Understanding Bacteremia and Sepsis:
Risk Factors in the Geriatric Population:
Prevention Strategies:
Early Detection:
Treatment Approaches:
Challenges in Managing Bacteremia and Sepsis in Older Adults:
Long-Term Outcomes and Follow-Up:
Here are some valuable resources to help you navigate the journey of caring for a loved one with bacteremia or sepsis:
| Resource | Description | Website |
|---|---|---|
| Sepsis Alliance | Provides information, support, and advocacy for sepsis patients and caregivers. | sepsis.org |
| Centers for Disease Control and Prevention (CDC) | Offers detailed information on sepsis, prevention, and treatment. | cdc.gov/sepsis |
| National Institute on Aging (NIA) | Provides resources on aging, health conditions, and caregiving. | nia.nih.gov |
| Family Caregiver Alliance | Offers support, education, and resources for family caregivers. | caregiver.org |
| American Geriatrics Society (AGS) | Provides information on geriatric health and care. | americangeriatrics.org |
Remember: You are not alone in this journey. Reach out to these resources, healthcare providers, and support networks to get the help and information you need.
By staying informed and proactive, you can significantly improve the health and well-being of your elderly loved one. Your care, attention, and compassion are invaluable in their recovery and quality of life.
Bloodstream infections in older patients
Challenges with Diagnosing and Managing Sepsis in Older Adults
Atypical Presentation of Bacteremia in Older Patients Is a Risk Factor for Death
Common Infections in Older Adults
Bacteraemia and quick Sepsis Related Organ Failure Assessment (qSOFA)
Introduction to Bacteremia, Sepsis, and Septic Shock
Insights into Severe Sepsis in Older Patients: From Epidemiology to Evidence-Based Management
Infection Control Issues in Older Adults
Sepsis: Diagnosis and Management
Antimicrobial Treatment Duration in Sepsis and Serious Infections
Early Recognition and Management of Sepsis in Adults: The First Six Hours
Evaluation and management of suspected sepsis and septic shock in adults
The critically ill older patient with sepsis: a narrative review
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.