
Recognizing and Treating Common End of Life Symptoms
Guide to Recognize and Treat Common End of Life Symptoms provides tips on managing symptoms experienced by those at the end of their lives – Topics such as pain, shortness of breath, respiratory distress, and anxiety, and provides suggestions for medications and complementary therapies to help manage these symptoms.
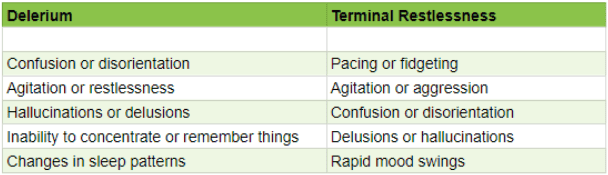
Delirium vs Terminal Restlessness
As an experienced hospice nurse, I understand how difficult it can be to distinguish between delirium and terminal restlessness. Both conditions can cause significant distress for the patient and their loved ones, and nurses must be able to tell the difference between them to provide the best possible care. In this article, I will share my knowledge and experience to help new hospice nurses understand the differences between delirium and terminal restlessness and how to rule out delirium.

The Importance of Documenting Hospice Visits at the Bedside
Our primary focus for our patients is comfort at the end of life as hospice nurses. We work tirelessly to ensure that our patients receive the best possible care during their end-of-life journey. An aspect of that care that is often overlooked, but incredibly important is timely documentation.
Documenting hospice visits at the bedside is crucial for several reasons. Not only does it help ensure that our patients are receiving the best possible care, but it also helps the hospice team as a whole and reduces issues when the caregiver must be involved in triage services. Here are just a few reasons why documenting hospice visits at the bedside is so important:
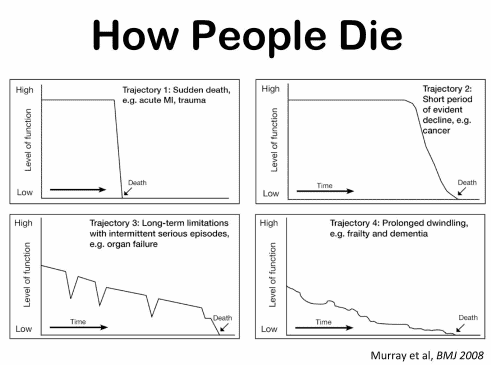
End-of-Life Determinations for Newly Admitted Patients
Admitting a patient to hospice services is a complex and sensitive process that requires careful assessment and communication. One of the challenges that hospice nurses face is to determine if the patient is close to the transitioning phase of dying, which is the final stage of life when death is imminent. This phase usually lasts for one to two weeks, and it is essential to prepare the family and provide a plan for increased hospice involvement during this time. However, on admission, hospice nurses do not have the luxury of having visited with the patient over the past several weeks to months to observe the changes that often signal that death is approaching. Therefore, they need to rely on other indicators to help them identify whether the patient is transitioning.
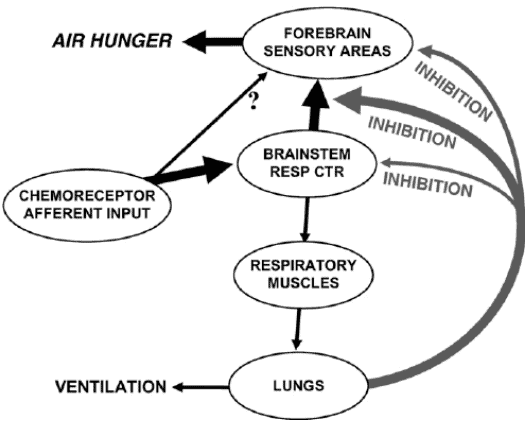
Air hunger management at end-of-life
I can count the times I’ve run into air hunger at the end of life as a visiting RN Case Manager for going on five years on one hand. Over the years, I’ve managed patients with pulmonary fibrosis, lung cancers (diverse types), breast cancer, COPD, congestive heart failure, B-cell lymphoma, leukemia, and other diseases that can impact one person’s ability to breathe correctly. Air hunger is rare in my firsthand experiences, but it can happen.
Air hunger often sounds like the person is gasping for breath without regard to the actual respiratory rate (how fast they are breathing); it can also sound like stridor (YouTube videos below where you can hear the difference).

Liquifying Ativan pills for easier delivery
Ativan, generically called Lorazepam, pills can be easily melted into liquid, and given to your loved one in a syringe. This is typically done vs. putting the pill under the tongue if your loved one has a dry mouth, and the Ativan pills are not melting under the tongue.
The process of melting lorazepam into a liquid will require the following resources:

Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Naomi Feil is an expert in gerontology and the creator of validation therapy, which is a means of communicating and acknowledging the internal reality of patients with dementia. When properly utilized, validation therapy can enhance the quality of life of patients with dementia as well as reduce stress on the family and caregivers.
While Naomi Feil and her followers (of which the writer of this article may be considered one, at least in form) focus on using this method of communication to maintain health with the potential for a level of restorative health, I want to share how the concepts of this method can be used during times of crisis.

Interviewing and Observation as part of the assessment
There are observation and interviewing skills you can develop which will help you learn:
What could cause the current change in condition
Determining if a patient is having terminal restlessness
Determining if your patient is within two weeks or less of life to live
Knowing where your patient is in the dying process
While this article is primarily meant for new nurses, what I’m sharing is also valuable for family members and loved ones. Anyone with patience and love toward the person being observed and interviewed can hone and develop these skills.

Fall Reduction – Reducing Falls in Personal Care Homes and Private Homes
Falls among the elderly can have severe consequences, including hip fractures, which can be life-threatening. As an experienced hospice registered nurse case manager, I understand the importance of fall prevention, especially in private homes, personal care homes, and assisted living facilities. This article aims to provide practical tips for reducing falls in these settings by following the nursing process: assessment, diagnosis, planning, implementation, and evaluation.

General Inpatient (GIP) Level of Care for Hospice Explained
GIP, or General Inpatient Hospice, is an often misunderstood aspect of hospice care. Both hospital staff and families sometimes have misconceptions about GIP. Families may assume it’s readily available upon request, while hospital professionals may believe it allows patients to remain in the hospital indefinitely, even when death is weeks away. This article will clarify the basics of GIP for hospice, including eligibility requirements, doctor’s orders, care plans, documentation, and education. We’ll conclude with two real-life cases to illustrate these points.
Learning Psychosocial Skills as a Hospice Nurse
One of the hardest lessons to learn as a nurse, in my experience and opinion, is the psychosocial skills necessary to help patients and their families work towards their healthcare goals. These skills are applicable to every field. While I, myself, am still growing as a registered nurse (heading towards my 5th year at the time of writing this article), I would like to share with you some of the lessons learned. These lessons are based on real-life cases where I will present the scenario, what I did that worked, and what I internally thought of opposite scenarios.
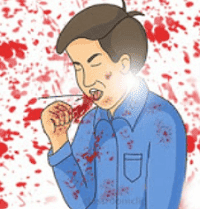
Coughing Up Blood (hemoptysis) Symptom Management
Hemoptysis, or coughing up blood, can be a distressing symptom for patients at the end of their life journey. As a hospice nurse, your expertise in managing this symptom is crucial in ensuring a peaceful and comfortable experience for your patients and their families.
