-
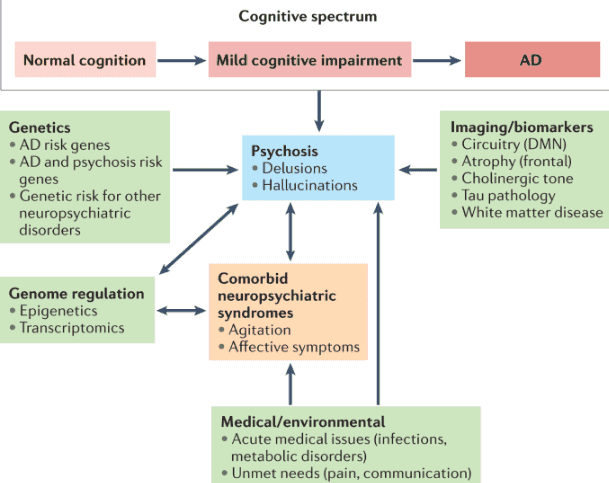
A Comprehensive Guide to Dementia-Induced Psychosis for Hospice Care Providers
This guide provides hospice nurses, caregivers, and family members with essential information on dementia-induced psychosis, including its signs, symptoms, differentiation from other conditions, and effective management strategies. -

Abdominal Aortic Aneurysm: A Life-Threatening Condition for Hospice Patients
The purpose of this article is to provide you with some information and guidance about AAAs and how they can be managed in hospice patients. -
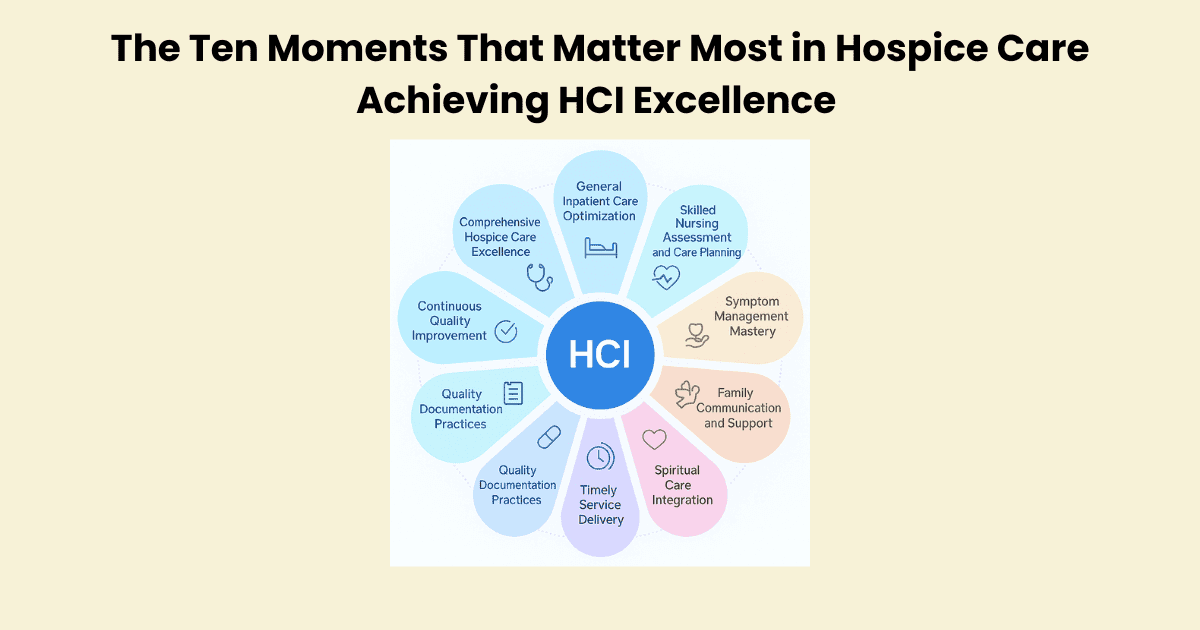
Achieving HCI Excellence: The Ten Moments That Matter Most in Hospice Care
Transform your hospice’s quality outcomes with Jose Escobar’s proven Polaris 10/10 HCI Execution Framework. This comprehensive guide reveals the ten critical moments that drive hospice excellence and offers practical strategies for executives and clinicians to achieve perfect HCI scores. -
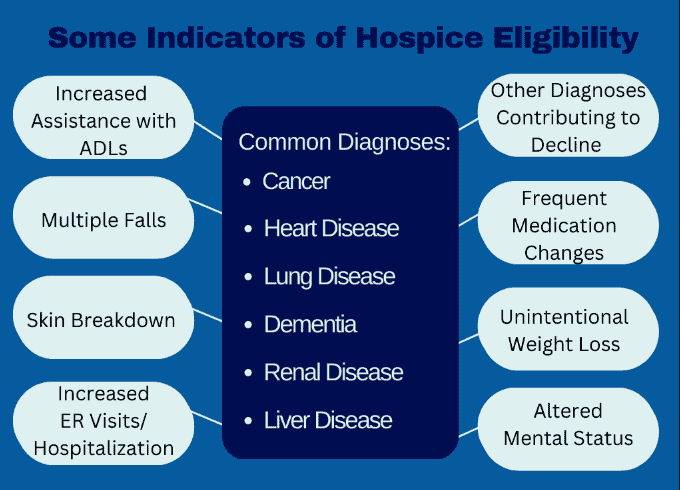
Admission Nurse: Essential Questions to Ask During the Hospice Admission Visit
As a hospice admission nurse, asking the right questions is crucial for assessing patients’ eligibility and providing compassionate care. This article explores critical questions to understand the patient’s condition, decline timeline, hospitalizations, functional abilities, cognitive status, and comorbidities. By gathering this information, nurses can support informed decisions, tailor interventions, and ensure a “good death” for patients and families. -

Adrenal Insufficiency Crisis Management for Terminally Ill Patients
Discover essential strategies for managing adrenal insufficiency crises in terminally ill patients. Learn about symptoms, risk factors, and crucial interventions to ensure patient comfort and safety. This guide provides valuable insights for hospice nurses and caregivers in this critical condition. -
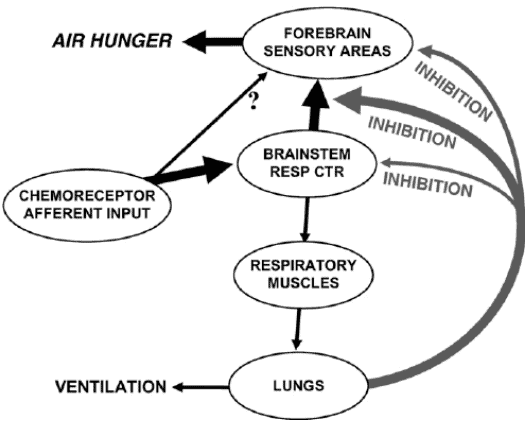
Air hunger management at end-of-life
I can count the times I’ve run into air hunger at the end of life as a visiting RN Case Manager for going on five years on one hand. Over the years, I’ve managed patients with pulmonary fibrosis, lung cancers (diverse types), breast cancer, COPD, congestive heart failure, B-cell lymphoma, leukemia, and other diseases that can impact one person’s ability to breathe correctly. Air hunger is rare in my firsthand experiences, but it can happen. Air hunger often sounds like the person is gasping for breath without regard to the actual respiratory rate (how fast they are breathing); it can also sound like stridor (YouTube videos below where you can hear the difference). -

Aromatherapy for Life’s Challenges: Supporting Anxiety, Grief, Loss, and End-of-Life Care
Explore how aromatherapy and essential oils relieve anxiety, grief, loss, and critical symptoms like pain and nausea across all stages of life. Practical, safe use tips are provided for caregivers, doulas, and health professionals to support holistic well-being. -

Assessing pain in non-verbal patients
Pain is a subjective sensation that can affect a person’s physical, emotional, and spiritual well-being. While pain can be measured objectively by using vital signs such as temperature, pulse, blood pressure, and respiration count, these indicators may not reflect the true intensity of pain that a person is experiencing. This is especially true for non-verbal patients, who cannot communicate their pain verbally. Non-verbal patients may include those with advanced dementia, terminal illness, or other conditions that impair their speech. In this article, I will discuss the importance of assessing pain in non-verbal patients, the tools and methods that can be used to do so, and the benefits of providing adequate pain relief for these patients. -
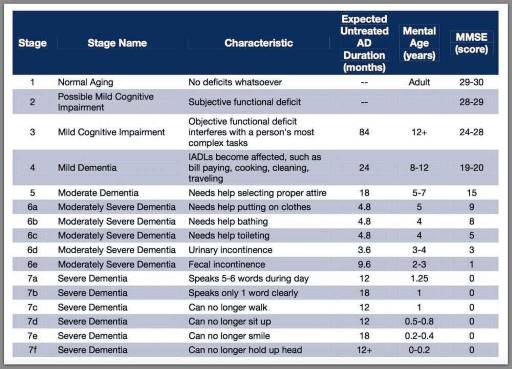
Assessing Patients on the FAST Scale: A Guide for Nurses
As a nurse who has cared for many terminally ill individuals with Alzheimer’s disease over the years, I understand the importance of accurately assessing their functional decline using the Functional Assessment Staging Tool (FAST). The FAST scale provides valuable information about the progression of Alzheimer’s disease and helps guide appropriate care planning for patients and their families. In this guide, I will walk you through the process of assessing patients on the FAST scale, starting from stage 1 and discussing when to stop reading the scale for determination. I will also provide three examples of patients at various stages of the FAST scale. -

Avoiding Problematic Language in Hospice Nursing Narratives
Proper documentation is crucial for hospice nurses to ensure Medicare compliance and maintain the patient’s eligibility for services. Auditors, who may not have a healthcare background, review these documents to determine if the patient’s condition is terminal. To avoid having the patient removed from service due to improper documentation, hospice nurses should be mindful of the words and phrases they use in their nursing narratives and progress notes. This article will guide what to avoid and why it is essential to paint a picture of a terminally ill patient. -
Balancing Patient Care and Compliance: The Impact of Extended Hospice Care for Dementia Patients
Explore how extended hospice care for dementia patients benefits families and saves Medicare money despite regulatory challenges around six-month prognosis rules. -

Best Practices for Approaching Combative Dementia Patients
Dementia is a progressive brain disorder that affects a person’s cognitive abilities, memory, and behavior. In the later stages of the disease, some patients can become combative and aggressive, making it difficult for caregivers to provide the necessary care. As a hospice nurse, it’s important to know how to approach and manage combative dementia patients to ensure their comfort and safety. Here are some best practices to consider: -

Boosting Hospice CAHPS Scores: The Power of Caregiver Training
This article delves into the transformative role of caregiver training in boosting Hospice CAHPS scores. Drawing on recent studies and expert insights, we explore practical strategies for enhancing caregiver education, ultimately leading to improved patient care and higher satisfaction ratings. -

Bowel Management for the Terminally Ill: A Guide for Caregivers and Hospice Nurses
Managing bowel problems in terminally ill patients is crucial for their comfort and dignity. This guide offers practical tips for caregivers and hospice nurses to address constipation, diarrhea, bowel obstruction, and ascites, ensuring patients’ better quality of life. -
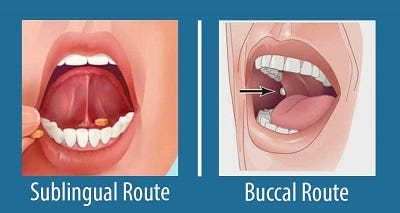
Buccal vs Sublingual for Liquid Medications
Your dying patient has lost their gag reflex as part of the dying process. One of the questions I implore you to ask yourself is what’s the safest route to administer liquid medications? Well, before even going to answer this question, unless contraindicated, make sure the patient’s head of the bed is at least at a 30 to 45-degree angle (I prefer the latter). The buccal route is the safest route to administer liquid medications at the end of life in my experience. In practice, I strongly encourage you as well as the families we mutually teach to give any liquid medications on the side of the mouth least likely to have spillage — this depends on the position of the patient — and slowly over time giving the medication in 0.25 ml increments allowing for the absorption of the medication switching cheeks as applicable.