The Unsung Heroes of Healthcare: How Palliative Care Nurses Transform Patient Care Beyond Terminal Diagnoses
Published on July 11, 2025
Updated on December 19, 2025
Published on July 11, 2025
Updated on December 19, 2025
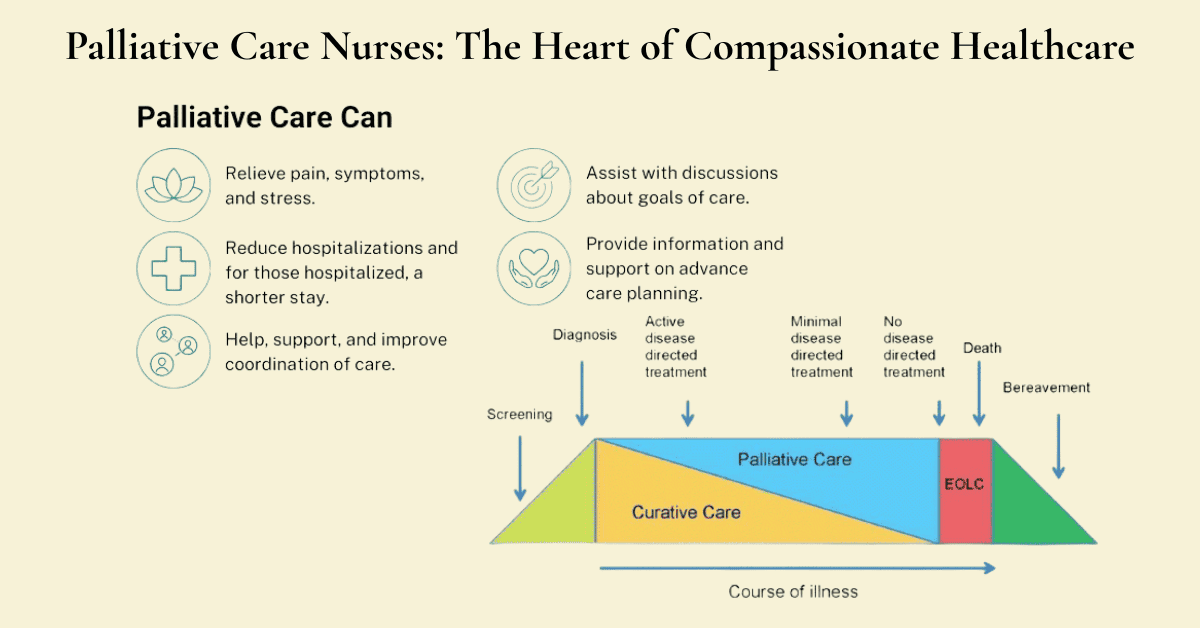
Table of Contents
When most people hear “palliative care,” they immediately think of hospice or dying patients. This widespread misconception creates barriers that prevent countless patients from receiving comfort care that could dramatically improve their quality of life. The truth is far different – palliative care is about living better with serious illness, and nurses are leading the transformation of how we understand and deliver this essential care.
This persistent myth stems from the historical connection between palliative care and hospice services. Still, it’s creating real harm for patients who could benefit from comfort care much earlier in their illness journey.
Breaking Down the Most Damaging Myths
The most significant barrier to accessing palliative care isn’t medical complexity or cost – it’s misunderstanding. Three myths cause the most damage:
Myth 1: “Palliative care means giving up hope” – In reality, palliative care supports hope by helping patients live as fully as possible with their condition. Patients receiving palliative care often have better symptom control and quality of life. Hope simply gets redefined from “cure at all costs” to “living well with illness.”
Myth 2: “You can only receive palliative care if you’re dying” – This couldn’t be further from the truth. Palliative care is appropriate at any stage of a serious illness and can be provided alongside curative treatments. Early integration often leads to better outcomes for patients and families.
Myth 3: “Palliative care is the same as hospice” – While hospice is a type of palliative care, palliative care is much broader. Hospice typically requires a prognosis of six months or less, but palliative care has no time restrictions and focuses on comfort regardless of prognosis.
The Real Impact of These Misconceptions
These misunderstandings create significant barriers that hurt both patients and the healthcare system. Late referrals mean patients suffer unnecessarily from uncontrolled symptoms, while emergency visits raise healthcare costs. Provider hesitation leads to missed opportunities for improved quality of life, while family resistance increases caregiver burden and stress. Patient fear causes people to avoid beneficial treatments, leading to poor care coordination.
The Clinical Practice Guidelines for Quality Palliative Care emphasize that palliative care is beneficial at any stage of a serious illness and can be provided along with treatments of curative or life-prolonging intent. This fundamental principle challenges the traditional view that comfort care and curative care are mutually exclusive.
Healthcare is evolving rapidly, and with it, our understanding of what it means to provide truly patient-centered care is also changing. Comfort care is expanding beyond traditional boundaries and becoming integrated into all aspects of healthcare delivery.
What Modern Comfort Care Actually Looks Like
Today’s comprehensive care approach recognizes that patients need support in all aspects of their care. Physical symptoms go far beyond just pain to include nausea, shortness of breath, fatigue, and sleep disturbances. Emotional and psychological needs encompass anxiety about the future, depression related to illness, grief over losses, and fear about uncertainty. Social concerns involve family dynamics, financial worries, work and role changes, and social isolation. Spiritual and existential questions include finding meaning in illness, connecting with faith or beliefs, exploring legacy and life review, and maintaining hope and purpose.
Integration Across All Healthcare Settings
Comfort care is no longer confined to specialized palliative care units. It’s becoming integrated across multiple healthcare settings in ways that would have been unimaginable just a decade ago.
Hospital-based integration now includes emergency departments recognizing palliative care needs and intensive care units incorporating comfort measures. These medical and surgical floors address symptom management, and outpatient clinics that provide ongoing support. Community-based expansion involves primary care practices offering basic palliative care skills, specialty clinics integrating comfort care, home health agencies providing palliative services, and long-term care facilities emphasizing comfort and quality of life.
The Evidence Supporting Early Integration
Research consistently shows that the early integration of palliative care leads to improved quality of life for patients and their families, better symptom management, reduced suffering, enhanced communication among patients, families, and healthcare teams, more appropriate healthcare utilization with fewer emergency visits, and lower healthcare costs without compromising care quality.
Nurses have always been at the heart of patient care, but their role in palliative care is particularly crucial. The nursing profession’s core values and skills align perfectly with the principles of palliative care, making nurses natural leaders in this expanding field.
The Nursing Advantage in Palliative Care
Holistic care perspective—Nurses are trained to see the whole person, not just the disease. This holistic approach is fundamental to effective palliative care, addressing physical comfort and symptom management, emotional support and coping, social relationships and family dynamics, and spiritual needs and meaning-making.
Continuous presence and availability – Nurses often spend extended time with patients and families, unlike other healthcare providers who may see patients briefly during rounds or appointments. This continuous presence allows them to build trusting relationships, observe subtle changes in condition, provide ongoing education and support, and coordinate care across disciplines.
Communication skills and advocacy – Nurses excel in therapeutic communication and patient advocacy, two essential components of palliative care. Their active listening helps them understand patient goals and preferences. Their empathetic presence provides emotional support during difficult times. Their ability to explain complex information clearly helps patients understand their condition and the available options. Their conflict-resolution skills facilitate family meetings and difficult conversations. Their cultural sensitivity ensures they respect diverse beliefs and practices.
Nurses as Essential Care Coordinators
The interdisciplinary nature of palliative care necessitates a central coordinator to ensure that all team members work together effectively. Nurses are ideally positioned for this role because they understand multiple disciplines. They work closely with physicians on medical management, collaborate with social workers on psychosocial needs, partner with chaplains on spiritual care, and coordinate with therapists on functional goals.
Nurses maintain continuity by following patients across various care settings, providing consistent communication with families, ensuring that care plans are implemented and updated, and bridging gaps between different healthcare providers. Most importantly, they focus on patient goals by keeping the patient’s wishes and preferences at the center of care decisions, advocating for patient autonomy and informed choice, helping families navigate complex healthcare decisions, and ensuring that care aligns with the patient’s values.
Growing Recognition of Nursing Leadership
Healthcare organizations increasingly recognize nurses’ vital role in palliative care leadership through specialized nursing roles, such as palliative care nurse practitioners, certified hospice and palliative nurses, palliative care clinical nurse specialists, and nurse case managers in palliative care programs. Educational initiatives include graduate programs in palliative care nursing, continuing education for all nurses in palliative care principles, certification programs for specialized palliative care nursing, and leadership development for nurse managers in palliative care.
Overcoming Challenges to Support Nursing Leadership
While nurses are well-positioned to lead palliative care initiatives, they face several challenges, including resource constraints from limited time due to high patient loads, insufficient staffing in many healthcare settings, and competing priorities and responsibilities. Educational gaps require more comprehensive palliative care education in nursing programs, ongoing training requirements for specialized skills, and access to continuing education opportunities. Organizational support needs include administrative backing of palliative care programs, integration of palliative care principles into organizational policies, and recognition and compensation for specialized palliative care nursing roles.
The future of palliative care depends on recognizing and supporting nurses’ unique contributions to this essential field. By understanding that palliative care is not just about dying but about living well with serious illness, and by empowering nurses to lead these initiatives, we can transform healthcare to be more compassionate, comprehensive, and truly patient-centered.
The biggest challenge facing palliative care today isn’t medical complexity or funding—it’s a simple misunderstanding about it. Too many people, including healthcare providers, still think palliative care equals “giving up” or means someone is dying soon. This couldn’t be further from the truth, and these misconceptions are preventing millions of patients from receiving care that could dramatically improve their quality of life.
Palliative care is specialized medical care focused on relieving the symptoms and stress of a serious illness, aiming to improve the quality of life for both the patient and their family. The Clinical Practice Guidelines for Quality Palliative Care define it as “an interdisciplinary care delivery system designed to anticipate, prevent, and manage physical, psychological, social, and spiritual suffering to optimize quality of life for patients, their families and caregivers.”
Comfort Care Versus Curative Care
One of the most persistent myths is that patients must choose between comfort care and curative care, but modern palliative care works alongside curative treatments to provide comprehensive support. Think of it this way: if someone has cancer and is receiving chemotherapy, palliative care can help manage the nausea, fatigue, and anxiety that come with treatment while the oncologist focuses on fighting the cancer. The patient gets the best of both worlds—aggressive treatment for their disease and expert management of symptoms and stress.
Palliative care addresses multiple dimensions of suffering that often get overlooked in traditional medical care. Physical symptoms include pain, shortness of breath, nausea, fatigue, and sleep problems. Emotional concerns encompass anxiety, depression, fear, and grief. Social challenges involve family stress, financial worries, work disruptions, and relationship changes. Spiritual questions encompass finding meaning in illness, connecting with one’s faith, and maintaining hope during challenging times.
The Spectrum of Palliative Interventions
Palliative care interventions range from simple comfort measures to complex medical management, all designed to improve quality of life. Basic interventions might include medication adjustments for better pain control, breathing techniques for anxiety, or helping families understand what to expect as an illness progresses. More complex interventions may involve specialized procedures to alleviate symptoms, coordination among multiple specialists, or intensive family counseling during complicated decision-making processes.
This comprehensive approach acknowledges that a serious illness impacts every aspect of a person’s life, not just their medical condition. The interdisciplinary team collaborates to address all these areas, ensuring patients receive comprehensive care supporting their overall well-being.
The timing of palliative care has evolved significantly over the past decade, with research consistently demonstrating that earlier integration yields better outcomes for patients and their families.
Early Integration with Treatment Plans
The old model of palliative care waited until curative treatments were exhausted, but evidence now shows this approach causes unnecessary suffering and missed opportunities. Modern palliative care begins at the time of diagnosis of a serious illness. It continues throughout the disease trajectory, whether that leads to cure, chronic illness management, or end-of-life care.
Research has shown that palliative care’s benefits are significant when it begins early. Patients report a better quality of life, improved symptom management, enhanced communication with their healthcare teams, and reduced anxiety and depression. Families experience less stress and feel more supported in their caregiving roles. Healthcare systems benefit from more appropriate resource utilization, fewer emergency department visits, and reduced overall costs, all without compromising the quality of care.
Concurrent Care Models
The most effective approach combines disease-directed treatment with palliative care from the outset, creating what is called a concurrent care model. In this approach, the oncologist continues chemotherapy while the palliative care team manages side effects and helps the family navigate difficult decisions. The cardiologist implants a device to support heart function while palliative care specialists address the patient’s depression and the family’s fears about the future.
This model recognizes that hope and comfort aren’t mutually exclusive. A patient can hope for a cure or disease control while also receiving expert help managing symptoms and stress. As the illness progresses, the balance might shift—perhaps less focus on aggressive treatments and more on comfort measures—but both elements remain present throughout the journey.
The key is understanding that palliative care intensity can be adjusted based on patient needs and disease progression. Early in an illness, palliative care might involve occasional consultations for symptom management and family support. As the disease advances, palliative care involvement typically increases, eventually becoming the primary focus if a cure is no longer possible.
Despite overwhelming evidence supporting palliative care, significant barriers prevent many patients from receiving these services when they could benefit most.
Addressing Provider Hesitation
Many healthcare providers hesitate to refer patients to palliative care because they worry it will destroy hope or signal that they’ve “given up” on their patients. This hesitation often stems from their own misunderstandings about the role and timing of palliative care. Some providers fear that discussing palliative care will damage their relationship with patients and families, while others simply lack knowledge about what palliative care services actually provide.
Education for healthcare providers is crucial for overcoming these barriers. Providers need to understand that referring patients to palliative care demonstrates comprehensive, patient-centered thinking rather than a failure of medical care. They need concrete examples of how palliative care can help their patients feel better and cope more effectively with treatment. Most importantly, they need to see palliative care as a partner in providing excellent care rather than a replacement for their own expertise.
Patient and Family Education Needs
Patients and families often resist palliative care because they associate it with dying or giving up hope. These fears are understandable, given how palliative care has been portrayed in the past; however, education can help families understand the real benefits. Effective education focuses on what palliative care can do rather than what it represents.
When explaining palliative care to patients and families, healthcare providers should emphasize practical benefits: better pain control, reduced nausea, improved sleep, help navigating the healthcare system, and support for family caregivers. They should provide concrete examples of how palliative care works in conjunction with other treatments and share success stories when appropriate.
The language used to describe palliative care matters enormously. Instead of saying “There’s nothing more we can do,” providers might say, “Let’s bring in our comfort care specialists to help you feel better while we continue your treatment.” Rather than “You need palliative care,” they could sa,y “I’d like you to meet with our team that specializes in helping people manage symptoms and stress during serious illness.”
Cultural sensitivity is essential when discussing palliative care, as different cultures have varying beliefs about illness, death, and medical decision-making. Some cultures prefer family-centered decision-making rather than individual autonomy, while others have specific rituals or practices that should be incorporated into care planning. Understanding and respecting these differences helps ensure that palliative care is truly patient and family-centered.
The goal is to help patients and their families understand that palliative care is about living as well as possible with a serious illness, regardless of the prognosis. When this message is communicated clearly and compassionately, most patients and families welcome the additional support and expertise that palliative care provides. The key is to time these conversations appropriately and ensure that all healthcare team members understand and support the palliative care approach.
By addressing these fundamental misunderstandings about palliative care, healthcare providers can help ensure that more patients receive the comprehensive, compassionate care they deserve throughout their illness journey. Understanding what palliative care really means, when it should begin, and how to overcome barriers to access creates the foundation for truly patient-centered care that addresses suffering in all its forms.
Palliative care nurses stand at the center of compassionate healthcare, serving as the bridge between medical expertise and human connection. Their role extends far beyond traditional nursing duties, encompassing the complex needs of patients facing serious illness and their families who are navigating one of life’s most challenging journeys. These dedicated professionals bring together clinical skills, emotional intelligence, and unwavering commitment to ensure that every patient receives comprehensive, dignified care regardless of their prognosis.
Continuous Presence and Accessibility
The foundation of effective palliative care nursing lies in the simple yet profound concept of being available. Unlike other healthcare providers who may see patients briefly during rounds or scheduled appointments, palliative care nurses maintain a continuous presence that becomes a source of comfort and security for patients and families. This availability isn’t just about physical presence—it’s about creating an environment where patients know someone is always there to listen, respond, and provide support when they need it most.
Continuous presence manifests in several essential ways. Nurses spend extended periods at the bedside, allowing them to observe subtle changes in a patient’s condition that might be missed during brief medical visits. They’re present during the quiet moments when patients may feel most vulnerable or when families need someone to talk through their fears and concerns. This extended contact time allows nurses to comprehensively understand each patient’s unique needs, preferences, and care goals.
The accessibility aspect extends beyond physical presence. Palliative care nurses make themselves emotionally and psychologically available to patients and families. They create safe spaces where people can express their deepest fears, ask difficult questions, and share their hopes without judgment. This emotional availability often proves just as necessary as any medical intervention, providing the human connection that helps patients maintain their dignity and sense of worth during illness.
Building Trust Through Consistent Availability
Trust forms the cornerstone of effective palliative care, and nurses build this trust through consistent, reliable availability. When patients and families know they can depend on their nurse to be there—whether for a medical concern, an emotional crisis, or simply to provide companionship during a difficult moment—it creates a foundation of security that enhances every aspect of care.
Consistency in availability means more than just showing up for scheduled shifts; it also involves being punctual and reliable. It involves maintaining reliable communication patterns, following through on promises, and being present during critical moments. When a nurse tells a patient they’ll check back in an hour, they do. When a family member calls with concerns, the nurse responds promptly and thoroughly to address their concerns. These seemingly small acts of reliability accumulate over time, creating a bond of trust that allows for more open communication and better care outcomes.
This trust-building process is particularly crucial in palliative care, as patients and their families often feel vulnerable and uncertain. They may have experienced disappointments with previous healthcare providers or feel overwhelmed by the complexity of their situation. Palliative care nurses who demonstrate consistent availability help restore faith in the healthcare system and create an environment where patients feel safe to express their true needs and concerns.
Serving as the Link Between Healthcare Teams
Palliative care nurses function as essential coordinators within the complex web of modern healthcare, serving as the vital link between various healthcare teams and ensuring that all aspects of patient care work together seamlessly. In today’s healthcare environment, patients often receive care from multiple specialists, each focusing on different aspects of their condition. Without effective coordination, this can result in fragmented care, conflicting recommendations, and confusion for patients and their families.
Nurses excel in this coordination role because they maintain continuous contact with patients and have a comprehensive understanding of their overall condition and needs. They work closely with physicians to ensure medical management aligns with patient goals, collaborate with social workers to address psychosocial concerns, partner with chaplains to provide spiritual support and coordinate with therapists to maintain functional abilities. This central coordination role ensures that all team members are working toward the same goals and that care plans are implemented consistently.
The coordination extends beyond the immediate healthcare team to include community resources, family caregivers, and other support systems. Palliative care nurses help connect patients with home health services, support groups, financial assistance programs, and other resources that can enhance their quality of life. They also work with family members to ensure they have the knowledge and skills to provide effective home care.
Bridging Communication Gaps Between Specialties
One of the most critical aspects of the coordination role involves bridging communication gaps between different medical specialties and healthcare disciplines. Each specialty tends to use its own terminology, focus on specific aspects of patient care, and operate according to its own timelines and priorities. This can lead to confusion and miscommunication, ultimately impacting patient care.
Palliative care nurses serve as translators and facilitators, helping ensure that information flows effectively between team members and that everyone understands the patient’s overall care plan. They attend interdisciplinary team meetings, participate in family conferences, and maintain ongoing communication with all involved providers. When conflicts arise between different treatment recommendations, nurses often help facilitate discussions to find solutions that align with patient goals and preferences.
This communication bridge extends to patients and families as well. Nurses help translate complex medical information into understandable terms, explain how different treatments and interventions fit together, and ensure that patients and families understand their options. They also communicate patient and family concerns back to the healthcare team, ensuring that the patient’s voice remains central to all care decisions.
Physical Symptom Assessment and Intervention
Palliative care nurses bring specialized expertise in comprehensive symptom assessment and management that goes far beyond basic nursing care. They’re trained to recognize and address the complex array of physical symptoms that can accompany serious illness, including pain, nausea, shortness of breath, fatigue, sleep disturbances, and many others. Their approach to symptom management is both systematic and individualized, recognizing that each patient’s experience is unique.
The assessment process involves not just identifying symptoms but understanding their impact on the patient’s overall quality of life. Nurses use validated assessment tools to measure symptom severity and track changes over time. They also consider how different symptoms interact with each other and how they affect the patient’s ability to participate in activities that are meaningful to them. This comprehensive assessment provides the foundation for developing effective intervention strategies.
Intervention strategies may include medication management, non-pharmacological comfort measures, environmental modifications, and patient and family education. Palliative care nurses are skilled in titrating pain medications, managing side effects, and implementing comfort measures like positioning, heat and cold therapy, and relaxation techniques. They also educate patients and their families about symptom management strategies that can be implemented independently, empowering them to take an active role in their care.
Emotional and Spiritual Support Integration
Recognizing that serious illness affects every aspect of a person’s being, palliative care nurses integrate emotional and spiritual support into their comprehensive care approach. They understand that physical symptoms cannot be effectively managed in isolation from emotional and spiritual distress, and they’re trained to address all these dimensions of suffering simultaneously.
Emotional support involves helping patients and families process the complex feelings that accompany serious illness, including fear, anger, sadness, and grief. Nurses provide a listening ear, validate emotions, and help patients develop coping strategies. They also recognize when patients might benefit from specialized mental health support and facilitate appropriate referrals. The emotional support extends to family members and caregivers, who often experience significant stress and may need guidance in managing their own emotional responses.
Spiritual support doesn’t necessarily involve religious practices, though it may include them when appropriate. Instead, it focuses on helping patients find meaning and purpose in their experiences, connect with what is most important to them, and maintain hope even in the face of serious illness. Nurses help patients explore their values, facilitate connections with spiritual care providers when desired, and support practices that bring comfort and peace.
Evidence-Based Practice Implementation
Palliative care nurses are committed to implementing evidence-based practices that ensure patients receive the most effective, up-to-date care available. This involves staying current with research findings, participating in continuing education, and continuously evaluating and improving their practice based on the latest evidence. They understand that effective palliative care requires both compassionate presence and clinical expertise grounded in solid research.
Evidence-based practice in palliative care encompasses a range of areas, including pain and symptom management protocols, communication strategies, family support interventions, and quality improvement initiatives. Nurses participate in research studies, contribute to quality improvement projects, and share their expertise with colleagues to advance the field. They also advocate for evidence-based policies and procedures within their organizations.
The implementation of evidence-based practice requires nurses to be critical thinkers who can evaluate research findings and apply them appropriately to individual patient situations. They must balance the latest research evidence with clinical expertise and patient preferences to provide truly patient-centered care. This approach ensures that patients receive not only compassionate care but also care that has been proven to be effective in improving outcomes and quality of life.
The pivotal role of palliative care nurses encompasses far more than traditional nursing duties. Through their continuous availability, coordination expertise, and holistic approach to symptom management, they create an environment where patients and families can navigate serious illness with dignity, comfort, and support. Their unique position within the healthcare team enables them to address the complex, interconnected needs of patients facing life-limiting conditions while ensuring that care remains focused on what matters most to each individual patient and their family.
Palliative care nursing requires a specialized set of skills that go far beyond traditional nursing competencies. These nurses must master complex communication techniques, develop expertise in comprehensive symptom management, and become skilled advocates for patients and their families as they navigate one of life’s most challenging journeys. The competencies required are both deeply clinical and profoundly human, demanding technical excellence alongside exceptional emotional intelligence and cultural awareness.
Difficult Conversation Facilitation
Palliative care nurses often find themselves at the center of some of the most challenging conversations in healthcare. They must be skilled in facilitating discussions about prognosis, treatment options, goals of care, and end-of-life preferences. These conversations require careful preparation, timing, and sensitivity to the emotional responses of those involved. Effective facilitation consists of creating a safe space where patients and their families can express their fears, hopes, and concerns without judgment. Nurses learn to use open-ended questions, reflective listening, and silence as therapeutic tools. They become adept at recognizing when someone needs time to process information and when to guide conversations toward important decisions gently. The ability to break down complex medical information into understandable terms while maintaining hope and dignity becomes essential. Nurses also learn to navigate situations where family members disagree about care decisions or when patients and families have different perspectives on treatment goals.
Family Conference Leadership
Leading family conferences represents one of the most complex communication skills in palliative care nursing. These meetings bring together multiple family members, healthcare providers, and sometimes friends or spiritual advisors to discuss care plans and make crucial decisions. Nurses must orchestrate these gatherings with skill and sensitivity, ensuring all voices are heard while keeping discussions focused and productive. Preparation involves understanding family dynamics, identifying key decision-makers, and anticipating potential conflicts or emotional responses. During conferences, nurses facilitate introductions, establish ground rules, and guide the flow of information sharing. They help translate medical terminology, clarify treatment options, and ensure patient preferences remain central to all discussions. Nurses use mediation skills when conflicts arise to help families find common ground and make decisions that honor the patient’s values and wishes.
Cultural Sensitivity in Care Discussions
Cultural competence in communication requires understanding how different cultures approach illness, death, and medical decision-making. Palliative care nurses must be aware of varying beliefs about pain expression, family involvement in care decisions, spiritual practices, and end-of-life rituals. Some cultures prioritize family-centered decision-making over individual autonomy, while others have specific protocols for discussing serious illness or death. Nurses learn to assess cultural preferences early in relationships and adapt their communication style accordingly. This might involve working with interpreters, incorporating traditional healing practices, or modifying care plans to respect religious observances. Cultural sensitivity also means recognizing one’s own cultural biases and assumptions while remaining open to learning from patients and families about their unique perspectives and needs.
Pain and Comfort Measures
Pain assessment and management in palliative care require sophisticated clinical skills and a comprehensive understanding of both pharmacological and non-pharmacological interventions. Nurses must be experts in using various pain assessment tools, understanding different types of pain, and recognizing how pain affects overall quality of life. They become skilled in medication titration, understanding opioid pharmacology, and managing side effects. Beyond medications, nurses implement comfort measures such as positioning, heat and cold therapy, massage, relaxation techniques, and environmental modifications. They understand that pain is subjective and multidimensional, affecting physical, emotional, social, and spiritual well-being. Effective pain management requires ongoing assessment, adjustment of interventions, and education of patients and families about pain control strategies they can implement independently.
Psychosocial Symptom Recognition
Palliative care nurses develop expertise in recognizing and addressing the psychological and social symptoms that accompany serious illness. This includes identifying signs of depression, anxiety, grief, and adjustment disorders that may not be immediately obvious. Nurses learn to assess for symptoms such as sleep disturbances, changes in appetite, social withdrawal, difficulty concentrating, and emotional lability. They understand how physical symptoms can contribute to psychological distress and vice versa. Recognition involves careful observation, therapeutic communication, and the use of validated screening tools. Once identified, nurses coordinate appropriate interventions, which may include counseling, support groups, spiritual care, or psychiatric consultation. They also provide ongoing emotional support and help patients and families develop coping strategies for managing psychological symptoms.
Quality of Life Optimization
Quality of life optimization requires nurses to understand what matters most to each individual patient and family. This involves a comprehensive assessment of functional status, symptom burden, social relationships, spiritual well-being, and personal goals. Nurses work with patients to identify activities and experiences that bring meaning and joy, then develop strategies to support these priorities within the constraints of illness. This may involve coordinating special events, facilitating meaningful conversations, or adjusting care routines to accommodate individual preferences. Quality of life optimization also includes helping patients maintain independence and dignity for as long as possible, supporting their roles within families and communities, and ensuring that care plans reflect individual values and preferences rather than standardized protocols.
Ensuring Patient Preferences Are Honored
Patient advocacy in palliative care means ensuring that the patient’s voice remains central to all care decisions, even when that voice becomes difficult to hear or interpret. Nurses become skilled at eliciting and documenting patient preferences about treatment options, care settings, and end-of-life wishes. They help patients understand their options and the implications of different choices, supporting informed decision-making without imposing their own values or judgments. When patients can no longer speak for themselves, nurses advocate for previously expressed wishes and collaborate with families to make decisions that are consistent with the patient’s known values. This advocacy extends to ensuring that care plans accurately reflect patients’ preferences regarding pain management, spiritual care, family involvement, and end-of-life rituals. Nurses also advocate for patient comfort and dignity in all care settings, challenging practices or policies that don’t serve the patient’s best interests.
Navigating Healthcare System Complexities
The healthcare system can be overwhelming and confusing for patients and families dealing with serious illness. Palliative care nurses become expert navigators, helping patients and families understand insurance coverage, access appropriate services, and coordinate care across multiple providers and settings. They help families understand the differences between palliative care and hospice, explain insurance benefits and limitations, and connect patients with community resources. Navigation also involves assisting families in understanding hospital policies, discharge planning processes, and options for care in various settings. Nurses advocate for appropriate referrals, timely access to services, and coordination between different healthcare teams. They also help families understand their rights as patients and how to access additional support when needed.
Supporting Informed Decision-Making
Supporting informed decision-making requires nurses to ensure that patients and their families have the necessary information to make choices that align with their values and goals. This involves presenting information in clear and understandable terms, checking for comprehension, and allowing time for questions and reflection. Nurses help patients and families understand the benefits and burdens of different treatment options, including the option of comfort-focused care. They facilitate discussions about prognosis and help families understand what to expect as the illness progresses. Supporting informed decision-making also means respecting the right to refuse information or delegate decision-making to others, particularly in cultures where family-centered decision-making is the preferred approach. Nurses ensure that decisions are made without coercion and that patients and families feel supported regardless of the choices they make.
The core competencies of palliative care nursing represent a sophisticated blend of clinical expertise, communication skills, and advocacy abilities. These competencies enable nurses to provide comprehensive, compassionate care that addresses the complex needs of patients and families facing serious illness. Mastering these skills requires ongoing education, practice, and reflection, as well as support from colleagues and organizations. When nurses develop and maintain these competencies, they become powerful advocates for patient-centered care and essential members of interdisciplinary teams working to improve the quality of life for those facing life’s most challenging circumstances.
Despite their critical role in healthcare, palliative care nurses face significant challenges that can impact their ability to provide optimal care. These challenges stem from systemic issues within healthcare organizations, societal misconceptions about palliative care, and the inherently complex nature of caring for patients with serious illnesses. Understanding these obstacles is essential for developing solutions that support these dedicated professionals and improve patient outcomes.
Staffing Limitations in Healthcare Settings
One of the most pressing challenges facing palliative care nurses is inadequate staffing across healthcare settings. Many hospitals, nursing homes, and home health agencies operate with minimal staffing levels, making it challenging to provide the comprehensive, time-intensive care that palliative patients require. Unlike other nursing specialties, where tasks can be completed quickly, palliative care often involves extended conversations with patients and their families, complex symptom management, and coordination among multiple healthcare providers.
The nursing shortage affects all areas of healthcare, but palliative care feels the impact particularly acutely because these patients often have complex needs that require more time and attention. When nurses are responsible for too many patients, they may find themselves rushing through visits or unable to spend adequate time addressing emotional and spiritual concerns. This creates a frustrating situation where nurses know what their patients need but lack the time to provide it fully.
Staffing limitations also affect the availability of specialized palliative care nurses. Many healthcare organizations have only a few nurses trained in palliative care principles, resulting in bottlenecks when multiple patients require specialized attention simultaneously. This shortage means that general nurses without specialized training may be called upon to provide palliative care, potentially resulting in less optimal patient and family outcomes.
Balancing Multiple Patient Needs
Palliative care nurses often find themselves managing complex caseloads where each patient has unique and demanding needs. Unlike other nursing specialties where patients may have similar conditions and treatment protocols, palliative care patients present with diverse diagnoses, varying stages of illness, and different goals for their care. This diversity requires nurses to shift their approach and expertise constantly throughout their workday.
The emotional intensity of palliative care adds another layer of complexity to managing multiple patients. Nurses may move from supporting a family through end-of-life decisions to helping another patient manage pain, then to coordinating care for someone just beginning their palliative care journey. This emotional switching requires a significant amount of mental and emotional energy, and the cumulative effect can be overwhelming.
Time management becomes particularly challenging when dealing with unpredictable situations common in palliative care. A routine visit may be extended significantly if a patient experiences a crisis or if family members require extensive emotional support. While these extended interactions are often necessary and beneficial, they can disrupt carefully planned schedules and create stress for nurses trying to meet all their patients’ needs.
Limited Legitimacy in Some Healthcare Environments
Despite the growing evidence supporting palliative care’s benefits, some healthcare environments still view it as less important than curative treatments. This attitude can manifest in various ways, from inadequate funding for palliative care programs to dismissive comments from colleagues who don’t understand the specialty’s value. Palliative care nurses may find themselves constantly advocating for their patient’s needs and defending their role within the healthcare team.
The misconception that palliative care equals “giving up” persists among some healthcare providers, creating barriers to appropriate referrals and support. When other healthcare professionals don’t understand the role of palliative care, they may be reluctant to involve palliative care nurses in patient care or may undervalue their contributions to patient outcomes. This lack of understanding can lead to isolation and frustration for palliative care nurses who see the positive impact of their work but struggle to gain recognition from their peers.
Administrative support for palliative care programs varies widely across healthcare organizations. Some institutions have robust palliative care departments with adequate resources and strong leadership support, while others treat palliative care as an afterthought or luxury service. This inconsistency creates uncertainty for nurses working in the field and can limit career advancement opportunities.
Need for Specialized Training and Education
Palliative care nursing requires specialized knowledge and skills that go beyond basic nursing education. However, many nursing programs provide limited education about palliative care principles, leaving new graduates unprepared for the complexities of this specialty. This educational gap means that nurses interested in palliative care must seek additional training, often at their own expense and on their own time.
Continuing education opportunities for palliative care nurses vary significantly by geographic location and the level of employer support. Rural nurses may face particular challenges in accessing specialized training due to distance and limited local resources. Even when training is available, the cost and time commitment can be prohibitive for nurses already struggling with heavy workloads and limited resources.
The rapidly evolving nature of palliative care necessitates that nurses continually update their knowledge and skills. New research, medications, and treatment approaches require ongoing education, but many healthcare organizations provide insufficient support for this professional development. This creates a burden on individual nurses to stay current while managing their regular patient care responsibilities.
Handling Complex Ethical Dilemmas
Palliative care nurses regularly encounter ethical dilemmas that require careful consideration and often have no clear-cut answers. These situations may involve conflicts between patient autonomy and family wishes, questions about the appropriateness of certain treatments, or decisions about resource allocation. The complexity of these ethical issues can create significant stress for nurses who want to do what’s best for their patients but may be uncertain about the right course of action.
One common ethical challenge involves patients and families having different perspectives on treatment goals. A patient may express a desire to focus on comfort care while family members push for continued aggressive treatment. Palliative care nurses must navigate these conflicts while respecting patient autonomy and maintaining therapeutic relationships with all involved parties. This balancing act requires exceptional communication skills and emotional resilience.
Cultural and religious considerations add another layer of complexity to ethical decision-making in palliative care. Nurses must respect diverse beliefs about illness, death, and medical decision-making while ensuring that patients receive appropriate care. This may involve accommodating practices that conflict with standard medical protocols or helping families navigate conflicts between traditional beliefs and modern medical recommendations.
Supporting Families Through Difficult Decisions
Families facing serious illness often struggle with complex decisions about treatment options, care settings, and end-of-life preferences. Palliative care nurses play a crucial role in supporting families through these decisions, but this responsibility can be emotionally challenging and professionally demanding. Nurses must provide information and guidance while avoiding the appearance of pushing families toward particular choices.
The emotional toll of supporting grieving families can be significant for palliative care nurses. They witness profound suffering and loss regularly, and they often form close relationships with patients and families during vulnerable times. When patients die, nurses may experience their own grief while simultaneously supporting bereaved family members. This dual role of professional caregiver and fellow human being experiencing loss can be challenging to navigate.
Family dynamics can complicate decision-making processes and create additional stress for palliative care nurses. Disagreements between family members, long-standing conflicts, and complex relationships all influence how families approach medical decisions. Nurses may find themselves serving as mediators or counselors in addition to their medical responsibilities, requiring skills that may not have been part of their formal training.
Time constraints and heavy caseloads compound the challenge of supporting families. Ideally, nurses would have unlimited time to sit with families, answer questions, and provide emotional support. In reality, they must balance these essential activities with other patient care responsibilities, sometimes leaving families feeling rushed or unsupported during critical moments.
Despite these significant challenges, palliative care nurses continue to provide essential care because they understand the profound impact they can have on patients and families during life’s most difficult moments. Addressing these challenges requires systemic changes within healthcare organizations, improved education and training opportunities, and greater recognition of the value of palliative care. By acknowledging and working to overcome these obstacles, we can better support palliative care nurses and ensure that patients receive the compassionate, comprehensive care they deserve.
The challenges facing palliative care nurses are real and significant, but not insurmountable. With adequate support, resources, and recognition, these dedicated professionals can continue to transform healthcare by bringing compassion, expertise, and dignity to the care of patients with serious illnesses. Their work represents the best of nursing practice, and addressing the challenges they face benefits not only the nurses themselves but also the countless patients and families who depend on their care.
The evidence supporting nursing-led palliative care is overwhelming and continues to grow stronger each year. When nurses take the lead in coordinating and delivering palliative care services, the positive effects ripple through every aspect of the healthcare experience. Patients feel better, families cope more effectively, and healthcare systems operate more efficiently. This comprehensive impact demonstrates why investing in nursing leadership for palliative care isn’t just beneficial—it’s essential for creating a healthcare system that truly serves the needs of people facing serious illness.
Enhanced Quality of Life Measures
When nurses lead palliative care initiatives, patients consistently report higher quality-of-life scores across multiple measurement tools. These improvements aren’t just statistical—they represent real, meaningful changes in how patients experience their daily lives. Nursing-led palliative care programs show remarkable success in helping patients maintain their sense of dignity, purpose, and connection to what matters most to them. Patients report feeling more in control of their care decisions, better understood by their healthcare team, and more confident that their preferences are being honored. The holistic approach that nurses bring to palliative care means that quality of life improvements extend beyond just physical comfort to include emotional well-being, social connections, and spiritual peace.
Research consistently demonstrates that patients in nursing-led palliative care programs experience improved sleep quality, enhanced appetite, increased energy levels, and a greater ability to participate in meaningful activities. These improvements often occur even when the underlying disease continues to progress, highlighting the effectiveness of symptom management and emotional support in dramatically enhancing a person’s experience of living with a serious illness. The nursing focus on patient education and empowerment helps individuals develop more effective coping strategies and feel better prepared to navigate the challenges of their condition.
Reduced Symptom Burden
Nurses excel at comprehensive symptom assessment and management, significantly reducing the overall symptom burden that patients experience. Their continuous presence and detailed observation skills allow them to identify symptoms early, often before they become severe or distressing. This proactive approach means that pain, nausea, shortness of breath, anxiety, and other symptoms are addressed quickly and effectively, preventing the escalation that can dramatically impact quality of life.
The nursing approach to symptom management extends beyond medication administration to encompass environmental modifications, positioning techniques, breathing exercises, relaxation strategies, and other non-pharmacological interventions. This comprehensive toolkit enables nurses to tailor symptom management strategies to each patient’s unique needs, preferences, and circumstances. Patients in nursing-led programs report lower pain scores, fewer episodes of breakthrough symptoms, and better overall comfort throughout their illness journey.
Increased Patient Satisfaction
Patient satisfaction scores consistently show higher ratings when nurses lead palliative care teams. This increased satisfaction stems from the nursing profession’s emphasis on patient-centered care, therapeutic communication, and advocacy. Patients feel heard, respected, and valued when nurses coordinate their care, resulting in higher confidence in their healthcare team and greater overall satisfaction with their care experience.
The nursing focus on building relationships and maintaining continuous communication creates an environment where patients feel safe expressing their concerns, asking questions, and participating actively in their care decisions. This collaborative approach yields care plans that accurately reflect patients’ values and preferences, leading to increased satisfaction with treatment choices and outcomes. Families also report greater satisfaction when nurses lead palliative care efforts, appreciating the clear communication, emotional support, and coordination that nurses provide.
Decreased Caregiver Stress and Burden
Family caregivers often experience significant stress and burden when caring for a loved one with a serious illness. Nursing-led palliative care programs specifically address these challenges by providing family members with comprehensive support, education, and resources. Nurses recognize that family well-being directly impacts patient outcomes, so they dedicate time and energy to supporting the entire family system.
Caregivers in nursing-led programs report feeling more confident in their ability to provide care, better prepared for what to expect as the illness progresses, and more supported in their caregiving role. Nurses provide practical education about medication management, symptom recognition, and comfort measures that families can implement at home. They also offer emotional support, helping family members process their feelings and develop healthy coping strategies. This comprehensive support significantly reduces caregiver stress levels and helps prevent caregiver burnout.
Many nursing-led programs offer 24-hour availability, which provides families with peace of mind, knowing they can reach a knowledgeable professional whenever concerns arise. This accessibility reduces anxiety and helps families feel more secure in their ability to manage challenging situations. Regular check-ins and proactive communication from nurses help identify potential problems early, preventing crises that can overwhelm family caregivers.
Improved Understanding of Care Options
Nurses excel at patient and family education, helping caregivers understand the full range of care options available to their loved one. This education extends beyond simply explaining medical treatments to encompass discussions about care settings, support services, financial resources, and community programs. Families gain a comprehensive understanding of how different options align with their loved one’s goals and preferences.
The nursing approach to education is typically more accessible and understandable than traditional medical explanations. Nurses use plain language, visual aids, and repeated explanations to ensure that families truly comprehend their options. They also encourage questions and provide ongoing clarification as families process complex information. This thorough education empowers families to make informed decisions and feel confident in their choices.
Nurses also help families understand the progression of serious illness and what to expect at different stages. This anticipatory guidance helps families prepare emotionally and practically for changes in their loved one’s condition. Understanding what is normal and what requires immediate attention reduces family anxiety and helps them respond appropriately to various situations.
Enhanced Coping Mechanisms
Nursing-led palliative care programs specifically focus on helping families develop effective coping strategies for managing the emotional challenges of serious illness. Nurses are trained in therapeutic communication techniques and understand how to support families through grief, fear, anger, and other challenging emotions. They offer both individual and group support opportunities, enabling families to connect with others facing similar challenges.
The nursing emphasis on hope and meaning-making helps families find ways to maintain positive connections and create meaningful experiences despite the challenges of illness. Nurses help families identify their strengths, build on existing coping skills, and develop new strategies for managing stress and uncertainty. This support extends beyond the patient’s death to include bereavement services that help families adjust to life after loss.
Families in nursing-led programs report feeling more resilient and better able to handle the ups and downs of their loved one’s illness. They develop stronger communication skills, learn to work together more effectively as a caregiving team, and find ways to maintain their own well-being while providing care. These enhanced coping mechanisms benefit families not just during the illness but also in their long-term adjustment and healing.
Reduced Unnecessary Hospitalizations
One of the most significant benefits of nursing-led palliative care in the healthcare system is the dramatic reduction in unnecessary hospitalizations. Nurses’ expertise in symptom management, patient education, and care coordination helps prevent many of the crises that typically lead to emergency department visits and hospital admissions. Their proactive approach to identifying and addressing problems early ensures that issues are resolved within the community before they escalate to the point of requiring acute care.
Nursing-led programs’ continuous monitoring and support help patients and families feel more confident managing symptoms at home. When families know they have access to knowledgeable nurses who can guide them through difficult situations, they’re less likely to panic and seek emergency care for manageable problems. This confidence, combined with better symptom control and family education, significantly reduces the number of avoidable hospitalizations.
When hospitalizations do occur, nursing-led programs often result in shorter lengths of stay because nurses coordinate closely with hospital teams to ensure smooth transitions and appropriate discharge planning. The comprehensive care plans and detailed communication that nurses provide help hospital staff understand the patient’s goals and preferences, leading to more appropriate care decisions and faster discharges to the preferred care setting.
More Appropriate Resource Utilization
Nursing-led palliative care programs excel at matching resources to patient needs, ensuring that healthcare dollars are spent on interventions that truly benefit patients and families. Nurses’ holistic assessment skills help identify which services and supports will be most helpful for each individual situation. This targeted approach prevents waste while ensuring that patients receive the care they need.
The nursing focus on patient goals and preferences helps guide decisions on resource allocation. Instead of providing standard packages of services, nursing-led programs tailor resource utilization to what matters most to each patient and family. This individualized approach often yields more cost-effective care that better meets patients’ needs and preferences.
Nurses also excel at identifying and connecting patients with community resources that can supplement formal healthcare services. Their knowledge of local programs, support groups, volunteer services, and other community assets helps families access additional support without increasing healthcare costs. This comprehensive approach to resource utilization maximizes the benefit of both formal and informal support systems.
Improved Care Coordination
Perhaps one of the most valuable benefits of nursing-led palliative care in the healthcare system is the dramatic improvement in care coordination. Nurses naturally serve as the central hub for communication between different providers, ensuring that everyone involved in a patient’s care is working toward the same goals. This coordination prevents duplication of services, reduces conflicting recommendations, and ensures that care plans are implemented consistently across all settings.
The nursing emphasis on communication and relationship-building creates strong partnerships between different healthcare providers. Nurses facilitate regular team meetings, maintain detailed care plans, and ensure critical information is promptly shared with all relevant team members. This coordination is particularly valuable for patients who receive care from multiple specialists or who move between different care settings.
Nursing-led coordination also extends to the transition periods that are often most challenging for patients and families. Nurses ensure that discharge planning begins early, that receiving providers have all necessary information, and that patients and families understand what to expect in their new care setting. This comprehensive approach to care transitions reduces readmissions, prevents medical errors, and helps patients adjust more quickly to changes in their care.
The impact of nursing-led palliative care extends far beyond individual patient encounters, transforming entire healthcare systems. By improving patient outcomes, supporting families more effectively, and utilizing resources more efficiently, nursing leadership in palliative care establishes a model of healthcare that truly meets the needs of individuals facing serious illness. These benefits demonstrate why investing in nursing education, support, and leadership development for palliative care isn’t just good for patients—it’s essential for creating sustainable, effective healthcare systems that can meet the growing needs of our aging population.
The future of palliative care relies on establishing a robust foundation of skilled, knowledgeable nurses who can meet the increasing demand for compassionate end-of-life care. As our population ages and more people live with serious chronic illnesses, the need for palliative care expertise continues to expand. Building nursing capacity in this field requires a comprehensive approach that includes robust education programs, strong institutional support, and meaningful professional development opportunities.
Foundational Palliative Care Competencies
Every nurse working in palliative care needs a solid foundation of core competencies that enable them to provide safe, effective, and compassionate care. These foundational skills extend beyond basic nursing education to encompass specialized knowledge in pain management, symptom control, communication techniques, and family support strategies. The National Consensus Project for Quality Palliative Care has identified eight domains that form the foundation of palliative care practice: structure and processes of care, physical aspects of care, psychological and psychiatric aspects, social aspects, spiritual and existential aspects, cultural aspects, care of the patient nearing death, and ethical and legal aspects.
Physical care competencies encompass advanced pain assessment and management skills, an understanding of complex symptom interactions, knowledge of medication management in serious illnesses, and the ability to provide comfort measures that extend beyond traditional medical interventions. Nurses must understand how serious illness affects the body differently than acute conditions and how to adapt their care accordingly. Communication competencies involve learning how to have difficult conversations about prognosis and goals of care, facilitating family meetings, providing emotional support during crisis situations, and helping patients and families navigate complex healthcare decisions. These skills require practice and ongoing refinement throughout a nurse’s career.
Psychosocial and spiritual competencies encompass understanding grief and loss, recognizing signs of depression and anxiety in seriously ill patients, supporting family dynamics during stressful times, and respecting diverse cultural and spiritual beliefs about illness and death. Nurses also need to develop skills in ethical decision-making, understanding advance directives, supporting patient autonomy, and navigating conflicts between patient wishes and family expectations.
Continuing Education Opportunities
Palliative care is a rapidly evolving field, and nurses must stay current with new research, treatment approaches, and best practices. Continuing education opportunities come in many forms, including formal academic programs, online courses, professional conferences, and workplace training sessions. The End-of-Life Nursing Education Consortium (ELNEC) provides comprehensive training programs specifically designed for nurses working in palliative and end-of-life care. These programs cover core competencies and offer specialized tracks tailored to various practice settings.
Online learning platforms have made palliative care education more accessible than ever before. Nurses can access webinars, interactive modules, and virtual simulations that enable them to practice skills in a safe and controlled environment. Professional organizations, such as the Hospice and Palliative Nurses Association, offer extensive continuing education resources, including journals, webinars, and certification review courses. Conference attendance provides opportunities to learn about cutting-edge research, network with colleagues, and participate in hands-on workshops that enhance clinical skills.
Many healthcare organizations are developing internal education programs that combine online learning with mentorship and hands-on experience. These programs often include shadowing experienced palliative care nurses, participating in interdisciplinary team meetings, and gradually taking on more complex cases under supervision. The key is creating learning opportunities that are both accessible and relevant to nurses’ daily practice.
Specialty Certification Pathways
Professional certification demonstrates a nurse’s commitment to excellence in palliative care, providing formal recognition of specialized knowledge and skills. The Hospice and Palliative Credentialing Center offers several certification options for nurses at different career stages. The Certified Hospice and Palliative Nurse (CHPN) credential is available to registered nurses with a minimum of two years of experience in hospice or palliative care. This certification validates core competencies and requires ongoing continuing education to maintain.
Advanced practice nurses can pursue certification as Certified Hospice and Palliative Nurses (CHPN), which recognizes the specialized knowledge required for nurse practitioners and clinical nurse specialists working in this field. These advanced certifications require additional education and clinical experience beyond basic nursing preparation. Pediatric palliative care has its own certification pathway (CHPPN) that recognizes the unique skills needed to care for children with life-limiting conditions and their families.
The certification process typically involves meeting eligibility requirements, passing a comprehensive examination, and maintaining certification through continuing education. Many nurses find that pursuing certification helps them identify knowledge gaps, provides structure for their professional development, and increases their confidence in providing palliative care.
Administrative Backing for Palliative Care Programs
Strong administrative support is essential for building successful palliative care nursing programs. Healthcare organizations require leaders who understand the value of palliative care and are willing to invest in the necessary resources to support these programs. This support must come from the highest levels of the organization, including the board of directors, chief executive officers, and chief nursing officers.
Financial investment in palliative care programs demonstrates administrative commitment and includes funding for specialized staff positions, education and training programs, and necessary equipment and supplies. Organizations that truly support palliative care create dedicated positions for palliative care nurses, provide competitive compensation, and offer opportunities for career advancement within the specialty. Policy development is another crucial area where administrative support makes a difference. Organizations require clear policies and procedures that support the integration of palliative care across all departments and care settings.
Quality improvement initiatives backed by the administration help ensure that palliative care programs meet high standards and continuously improve their effectiveness. This includes regular evaluation of patient outcomes, family satisfaction surveys, and staff feedback about program effectiveness. Administrative support also involves advocating for palliative care at the organizational level, ensuring that these programs are included in strategic planning and resource allocation decisions.
Interdisciplinary Team Development
Effective palliative care relies on strong interdisciplinary teams that work collaboratively to address the complex needs of patients and their families. Building these teams requires intentional effort to recruit qualified professionals, provide team training, and create systems that support effective collaboration. Team composition typically includes physicians, nurses, social workers, chaplains, and other specialists as needed. Still, the key is ensuring that all team members understand their roles and how they contribute to comprehensive patient care.
Team training programs help team members learn to work together effectively, understand each other’s roles and areas of expertise, and develop shared approaches to patient care. This training should include communication skills, conflict resolution, and decision-making processes that ensure all voices are heard and respected. Regular team meetings provide opportunities for case discussion, care planning, and professional development that strengthen team cohesion and effectiveness.
Creating shared documentation systems and communication protocols helps ensure that all team members have access to the information they need to provide coordinated care. This includes electronic health records that support interdisciplinary documentation, secure messaging systems for team communication, and standardized care planning tools that facilitate collaboration.
Resource Allocation for Training
Building palliative care nursing capacity requires significant investment in training and education resources. Organizations must allocate sufficient funding for initial training programs that prepare nurses to work in palliative care settings. This includes both didactic education and hands-on clinical experience under the supervision of experienced mentors. Ongoing education budgets should support continuing education requirements, conference attendance, and certification maintenance.
Staffing considerations are crucial for supporting training programs. Organizations must provide adequate staffing levels that enable experienced nurses to serve as mentors and preceptors without compromising patient care. This may require hiring additional staff or adjusting patient assignments to accommodate training activities. Technology resources, including access to online learning platforms, simulation equipment, and educational materials, support the development of effective training programs.
Time allocation for training activities must be built into work schedules and job expectations. Nurses need protected time for education activities, and organizations must recognize that investing in training time leads to better patient outcomes and improved staff retention in the long term.
Mentorship Programs
Mentorship plays a crucial role in developing palliative care nursing expertise and supporting nurses throughout their careers in this challenging specialty. Formal mentorship programs pair experienced palliative care nurses with those new to the field, providing structured support and guidance during the transition to specialized practice. These relationships help new nurses develop clinical skills, learn to navigate complex ethical situations and build confidence in their ability to provide compassionate care.
Peer mentorship opportunities enable nurses at similar experience levels to support one another through shared learning experiences and collaborative problem-solving. This type of mentorship is particularly valuable for addressing the emotional challenges of palliative care work and preventing burnout. Reverse mentorship programs, where newer nurses share their fresh perspectives and technological skills with more experienced colleagues, create mutual learning opportunities that benefit everyone involved.
Effective mentorship programs include clear expectations and goals, regular check-ins between mentors and mentees, and structured activities that promote learning and professional growth. Organizations should provide mentors with training to help them develop effective coaching and teaching skills and recognize and reward them for their contributions to professional development.
Research and Evidence-Based Practice Integration
Palliative care nursing must be grounded in the best available evidence, and nurses need opportunities to participate in research activities and implement evidence-based practices in their daily work. Research participation can range from data collection for quality improvement projects to involvement in multi-site clinical trials that advance the field’s knowledge base. Nurses who participate in research develop critical thinking skills, learn to evaluate evidence and contribute to improving care for future patients.
Evidence-based practice initiatives enable nurses to learn how to identify clinical questions, search for relevant research, assess the quality of evidence, and implement practice changes based on research findings. These skills are essential for delivering high-quality palliative care and ensuring that patients receive interventions that have been proven effective. Journal clubs and research presentations provide forums for nurses to share research findings with colleagues and discuss how evidence can be applied in their practice settings.
Organizations should support research activities by providing access to research databases, funding for research projects, and time for nurses to participate in research activities. Partnerships with academic institutions can provide additional research opportunities and help bridge the gap between research and practice.
Leadership Development in Palliative Care
As palliative care continues to expand, there is a growing need for nurse leaders who can champion these programs and guide their development within healthcare organizations. Leadership development programs help nurses develop the skills needed to lead palliative care initiatives, manage interdisciplinary teams, and advocate for program resources and support.
Formal leadership training might include courses in healthcare management, quality improvement, financial planning, and organizational change. These skills are essential for nurses who want to advance into leadership positions within palliative care programs. Project leadership opportunities enable nurses to gain experience in leading quality improvement initiatives, developing new programs, and implementing practice changes.
Professional organization involvement offers nurses opportunities to develop leadership skills while contributing to the advancement of palliative care nursing. This might include serving on committees, presenting at conferences, or participating in policy development activities. Advanced education in areas like healthcare administration, education, or clinical specialization can prepare nurses for senior leadership roles in palliative care.
The goal of leadership development is to prepare nurses who can not only provide excellent direct patient care but also shape the future of palliative care nursing through program development, policy advocacy, and mentorship of the next generation of palliative care nurses.
Building palliative care nursing capacity requires a comprehensive approach that addresses education, institutional support, and professional development. By investing in these areas, healthcare organizations can ensure they have the skilled and knowledgeable nurses needed to provide compassionate, high-quality palliative care to patients and their families facing serious illness. The future of palliative care depends on our commitment to developing and supporting these essential healthcare professionals.
The time has come for decisive action to support palliative care nurses who serve as the backbone of compassionate healthcare. These dedicated professionals face significant challenges while providing essential care to patients and families during life’s most difficult moments. Supporting them requires commitment from healthcare organizations, collaboration among healthcare professionals, and active engagement from patients and families. Every stakeholder has a vital role to play in ensuring that palliative care nurses have the resources, recognition, and support they need to continue their life-changing work.
Investment in Training and Resources
Healthcare organizations must make substantial investments in palliative care nursing education and resources to build the necessary capacity to meet the growing demand. This investment begins with comprehensive orientation programs that prepare new nurses for the unique challenges of palliative care practice. Organizations should provide funding for specialized training programs, including the End-of-Life Nursing Education Consortium courses, certification preparation, and continuing education opportunities. Financial support for conference attendance, online learning platforms, and professional development activities demonstrates organizational commitment to nursing excellence.
Resource allocation must extend beyond education to include adequate staffing levels that allow nurses time to provide the comprehensive, relationship-based care that palliative patients require. Organizations need to invest in technology that supports palliative care delivery, including electronic health records designed for interdisciplinary communication, telehealth platforms for remote consultations, and mobile devices that enable nurses to document care and communicate with families efficiently. Physical resources such as comfort care supplies, symptom management equipment, and family support materials are equally essential investments.
Recognition of Nursing Contributions
Healthcare organizations must formally recognize the specialized expertise and significant contributions that palliative care nurses bring to patient care. This recognition should include competitive compensation packages that reflect the advanced skills and emotional demands of palliative care nursing. Career advancement opportunities within palliative care programs help retain experienced nurses and encourage others to develop expertise in this specialty. Organizations should create leadership positions for palliative care nurses, including clinical nurse specialist roles, program coordinator positions, and nurse manager opportunities.
Recognition also involves celebrating the achievements and impact of palliative care nurses through internal communications, awards programs, and professional development opportunities. Organizations should highlight success stories, patient outcomes, and family testimonials that demonstrate the value of nursing-led palliative care. Public recognition through community outreach, media coverage, and professional presentations helps elevate the profile of palliative care nursing and attracts new nurses to the field.
Integration of Palliative Care Principles
Healthcare organizations must integrate palliative care principles into their operations rather than treating them as add-on services. This integration begins with organizational policies that support early palliative care referrals, interdisciplinary collaboration, and patient-centered care planning. Quality improvement initiatives should incorporate palliative care metrics, and organizational strategic plans should prioritize developing and expanding palliative care.
Integration requires training all healthcare staff in basic palliative care principles, not just specialized palliative care teams. Primary care nurses, emergency department staff, intensive care nurses, and other healthcare workers should understand when and how to incorporate comfort care measures and communicate with palliative care specialists. Organizations should develop clear protocols for palliative care consultation, care transitions, and family communication that ensure consistent, high-quality care across all departments and settings.
Collaborative Care Approaches
Healthcare professionals across all specialties must embrace collaborative approaches that recognize palliative care nurses as essential partners in patient care. Physicians should view palliative care nurses as clinical experts who bring unique insights into symptom management, family dynamics, and patient preferences. Collaborative care means including nurses in medical decision-making, respecting their clinical assessments, and supporting their recommendations for patient care modifications.
Effective collaboration requires regular communication between healthcare team members, including participation in interdisciplinary rounds, family conferences, and care planning meetings. Healthcare professionals should develop standardized communication protocols that ensure important information flows efficiently between team members. This includes sharing assessment findings, treatment responses, and family concerns in a manner that supports coordinated care delivery.
Referral and Consultation Practices
Healthcare professionals must develop appropriate referral and consultation practices that ensure patients receive palliative care when they can benefit most. This involves understanding the distinction between palliative care and hospice care, identifying appropriate referral triggers, and making timely referrals that enable palliative care teams to establish meaningful relationships with patients and their families. Referral practices should be based on patient needs rather than prognosis, with early integration of palliative care for patients with serious illnesses.
Consultation practices should respect the expertise of palliative care nurses and include them in discussions about patient care goals, treatment options, and family support needs. Healthcare professionals should be prepared to implement palliative care recommendations and maintain ongoing communication with palliative care teams about patient responses to interventions. Clear documentation of consultation requests, suggestions, and follow-up plans ensures continuity of care and supports quality improvement efforts.
Continuing Education Participation
Healthcare professionals have a responsibility to participate in continuing education about palliative care principles and practices. This education helps them understand how to integrate comfort care measures into their routine practice, recognize when patients might benefit from specialized palliative care services, and communicate effectively with palliative care teams. Professional organizations should offer palliative care education opportunities, and healthcare professionals should actively seek out these learning experiences.
Continuing education should include training in difficult conversations, symptom assessment and management, cultural competency, and ethical decision-making in the context of serious illness. Healthcare professionals should also learn about the roles and expertise of different palliative care team members, including the specialized contributions of palliative care nurses. This education helps build respect for palliative care nursing and supports more effective collaboration.
Understanding Palliative Care Options
Patients and their families must actively participate in understanding palliative care options and advocating for comprehensive care that addresses all dimensions of suffering. This understanding begins with learning that palliative care is not just for people who are dying but is appropriate for anyone with a serious illness who could benefit from additional symptom management and support. Patients and families should ask their healthcare providers about palliative care services and request referrals when they believe these services could be helpful.
Education about palliative care should include understanding the roles of different team members, particularly the central role that nurses play in coordinating care and providing ongoing support. Patients and families should know that palliative care nurses are specially trained to address physical symptoms, emotional concerns, and family needs in ways that complement medical treatment. Understanding these roles helps patients and families know what to expect from palliative care services and how to work effectively with their care teams.
Advocating for Comprehensive Care
Patients and families must become advocates for comprehensive care that addresses their full range of needs and concerns. This advocacy involves clearly communicating their goals, preferences, and concerns to their healthcare teams. Patients should feel empowered to ask questions about their care options, express their values and priorities, and request modifications to their care plans when needed.
Advocacy also means speaking up when care doesn’t meet their needs or when they encounter barriers to accessing palliative care services. Patients and families should know their rights to request second opinions, ask for different providers, or seek care in other settings when their current care isn’t meeting their needs. They should also advocate for family members and friends who might benefit from palliative care but haven’t been offered these services.
Engaging with Healthcare Teams
Active engagement with healthcare teams is essential for receiving optimal palliative care. This engagement involves participating in care planning discussions, asking questions about treatment options, and providing feedback about the effectiveness of interventions. Patients and their families should prepare for healthcare visits by writing down questions, concerns, and observations about any symptoms or changes in quality of life.
Engagement also means building relationships with healthcare team members, particularly palliative care nurses who often serve as primary coordinators and advocates. Patients and families should communicate openly about their experiences, preferences, and concerns. They should also provide feedback on what is working well and what could be improved in their care. This ongoing communication enables healthcare teams to provide more personalized and effective care.
Moving Forward Together
Supporting palliative care nurses requires sustained commitment from all stakeholders in the healthcare system. Healthcare organizations must invest in the infrastructure, education, and recognition that palliative care nurses need to thrive. Healthcare professionals must embrace collaborative approaches that respect nursing expertise and integrate palliative care principles into routine practice. Patients and families must become informed advocates who actively engage with their healthcare teams and seek comprehensive care that addresses all their needs.
The future of healthcare depends on our collective commitment to supporting those who provide compassionate care during life’s most challenging moments. Palliative care nurses exemplify the best of healthcare, combining clinical expertise with compassionate care to enhance the quality of life for patients and their families facing serious illnesses. By supporting these essential healthcare professionals, we ensure that everyone facing serious illness receives the comprehensive, compassionate care they deserve.
The call to action is clear: we must work together to create healthcare systems that truly support palliative care nurses and enable them to provide the exceptional care that patients and families need. The time for action is now, and the responsibility belongs to all of us.
As we reach the end of our exploration into the world of palliative care nursing, one truth emerges crystal clear: palliative care nurses are not just healthcare providers—they are the embodiment of compassion in action. They represent the very best of what healthcare can be when it combines clinical expertise with genuine human connection. These remarkable professionals dedicate their careers to ensuring that no one faces serious illness alone, that suffering is minimized, and that dignity is preserved even in life’s most challenging moments.
The Heart of Healthcare Transformation
Palliative care nursing represents a fundamental shift in how we approach healthcare, from a system focused solely on curing disease to one that prioritizes the whole person and their quality of life. These nurses understand that healing doesn’t always mean curing and that sometimes the most significant medical intervention is simply being present with someone in their time of need. They bridge the gap between high-tech medical care and high-touch human compassion, proving that both are essential for truly effective healthcare.
The Clinical Practice Guidelines for Quality Palliative Care emphasize that palliative care is “an interdisciplinary care delivery system designed to anticipate, prevent, and manage physical, psychological, social, and spiritual suffering to optimize quality of life for patients, their families and caregivers.” Palliative care nurses are at the center of this comprehensive approach, serving as the coordinators, advocates, and constant presence that makes this vision a reality.
Beyond Traditional Nursing Roles
What makes palliative care nursing essential goes far beyond traditional nursing duties. These professionals master complex symptom management while simultaneously providing emotional support, spiritual care, and family education. They navigate difficult conversations about prognosis and goals of care while maintaining hope and dignity. They coordinate care between multiple specialists while ensuring the patient’s voice remains central to all decisions. This multifaceted role requires not only clinical expertise but also exceptional emotional intelligence, cultural competence, and effective communication skills.
Palliative care nurses also serve as translators, helping patients and their families understand complex medical information, explaining treatment options in clear and understandable terms, and ensuring that healthcare teams understand the patient’s preferences and values. They are advocates who fight for their patient’s wishes to be honored, educators who empower families to provide better care and counselors who help people process the most difficult experiences of their lives.
The Unique Value They Bring
The essential nature of palliative care nursing becomes clear when we consider what happens when these services are unavailable. Patients suffer from uncontrolled symptoms, families feel overwhelmed and unprepared, healthcare resources are used inefficiently, and people face serious illness without the comprehensive support they need and deserve. Studies consistently show that when palliative care nurses are involved in patient care, outcomes improve across every measure—pain control, quality of life, family satisfaction, healthcare utilization, and even survival in some cases.
These nurses bring a unique perspective to healthcare teams because they focus on what matters most to patients rather than what is most medically interesting. They ask different questions: “What does a good day look like for you?” “What are you most worried about?” “How can we help you maintain the relationships and activities that give your life meaning?” This patient-centered approach transforms not just individual care experiences but entire healthcare cultures.
Impact on Patient Care Quality
When we support palliative care nurses through adequate resources, education, and recognition, the benefits ripple outward in remarkable ways. Well-supported nurses deliver better patient care, resulting in improved outcomes and higher patient and family satisfaction. They’re able to spend adequate time with each patient, provide thorough education and support, and coordinate care more effectively. This comprehensive approach reduces emergency department visits, prevents unnecessary hospitalizations, and enables patients to remain in their preferred care settings for more extended periods.
The ripple effect extends to pain and symptom management, where supported nurses can implement evidence-based practices more effectively. They have the time to assess symptoms thoroughly, try multiple interventions, and work with patients to find the most effective approaches. This leads to improved comfort levels, enhanced quality of life, and a greater ability for patients to participate in meaningful activities and relationships.
Strengthening Healthcare Teams
Supporting palliative care nurses strengthens the entire healthcare team and organization. These nurses often serve as mentors and educators for other healthcare providers, sharing their expertise in communication, symptom management, and patient advocacy. When palliative care nurses are well-supported and recognized, they’re more likely to stay in their positions, building expertise and institutional knowledge that benefits everyone.
The collaborative approach that palliative care nurses bring to healthcare teams improves communication and coordination across disciplines. They help break down silos between specialties, facilitate better information sharing, and ensure that all team members are working toward the same patient-centered goals. This improved teamwork benefits not just palliative care patients but all patients served by these healthcare organizations.
Transforming Healthcare Culture
Perhaps the most significant ripple effect of supporting palliative care nurses is the transformation of the healthcare culture itself. These nurses model patient-centered care, compassionate communication, and holistic thinking that influences how other healthcare providers approach their work. They demonstrate that it’s possible to provide high-quality medical care while also attending to emotional, social, and spiritual needs.
When healthcare organizations invest in palliative care nursing, they send a clear message about their values and priorities. They demonstrate commitment to comprehensive, compassionate care that extends beyond just treating disease. This cultural shift attracts other healthcare providers who share these values, helping to create work environments where all staff can provide more meaningful and satisfying care.
Benefits for Families and Communities
The ripple effects of supporting palliative care nurses profoundly extend into families and communities. Well-supported nurses have more time and energy to provide comprehensive family education and support, which improves caregiving skills and reduces caregiver burden. Families who receive good palliative care support are better prepared for their caregiving roles, more confident in managing symptoms and crises, and more satisfied with their loved one’s care.
These benefits continue long after a patient’s death, as families who received good palliative care support often report better bereavement outcomes and fewer complicated grief reactions. They’re more likely to feel that their loved one received good care and that their own needs were recognized and addressed. This positive experience with healthcare during one of life’s most difficult times can influence how families approach healthcare decisions in the future.
Economic and System-Wide Benefits
Supporting palliative care nurses also creates significant economic benefits for healthcare systems and society. Well-supported palliative care programs reduce healthcare costs through more appropriate resource utilization, fewer emergency department visits, shorter hospital stays, and better care coordination. These savings can be reinvested in other healthcare priorities, creating a positive cycle of improvement.
The system-wide benefits include reduced burnout among healthcare providers, improved staff retention, and better recruitment of high-quality professionals. Healthcare organizations with robust palliative care programs often become employers of choice for nurses and other healthcare professionals seeking to work in environments that prioritize comprehensive, compassionate care.
A Call for Sustained Investment
Moving forward requires sustained investment in palliative care nursing at every level—from individual healthcare organizations to national policy initiatives. This investment must include adequate funding for education and training programs, competitive compensation that reflects the specialized skills required, and ongoing support for professional development and career advancement. Healthcare organizations must recognize that investing in palliative care nursing is not just the right thing to do—it’s a wise business decision that improves outcomes while reducing costs.
Investment also means creating work environments that support palliative care nurses in their challenging roles. This includes adequate staffing levels that allow time for the relationship-building and comprehensive care that palliative patients require, access to mental health support and stress management resources, and recognition programs that acknowledge the unique contributions these nurses make to patient care and organizational success.
Building for the Future
As our population ages and more people live with serious chronic illnesses, the need for palliative care expertise will only continue to grow. We must build educational pipelines that prepare the next generation of palliative care nurses while supporting current nurses in developing advanced skills and leadership capabilities. This includes expanding palliative care content in nursing school curricula, creating more residency and fellowship programs for new graduates, and providing ongoing continuing education opportunities for practicing nurses.
Building for the future also means embracing innovation and technology that can enhance the delivery of palliative care. This includes telehealth platforms that extend the reach of palliative care into rural and underserved communities, electronic health records that support interdisciplinary communication and care coordination, and mobile technologies that help patients and their families manage symptoms and communicate with their care teams.
Creating Sustainable Change
Sustainable change requires commitment from all stakeholders in the healthcare system. Healthcare leaders must champion palliative care as an essential component of high-quality healthcare, not an optional add-on service. Policymakers must support legislation and regulations that promote access to palliative care and adequate reimbursement for these services. Professional organizations must continue to advocate for palliative care nursing and provide resources for education and professional development.
Perhaps most importantly, we must continue to educate the public about palliative care and how it can benefit anyone facing a serious illness. This education helps reduce the stigma and misconceptions that prevent people from accessing palliative care when they could benefit most. It also helps families understand how to advocate for comprehensive care that addresses all their needs and concerns.
The Moral Imperative
Ultimately, supporting palliative care nurses is a moral imperative that reflects our values as a society. These nurses represent our commitment to treating every person with dignity and compassion, regardless of their prognosis or ability to be “cured.” They embody our belief that suffering should be relieved whenever possible and that no one should face serious illness alone.
The work of palliative care nurses reminds us that healthcare is fundamentally about human relationships and that the most powerful healing often comes not from medications or procedures but from the presence of someone who truly cares. In a healthcare system that can sometimes feel impersonal and technology-driven, palliative care nurses preserve the human element that makes healthcare truly healing.
Our Shared Responsibility
As we move forward, we all share responsibility for supporting palliative care nurses and ensuring that their essential work continues and expands. Healthcare organizations must invest in these programs and recognize their value. Healthcare providers must embrace palliative care principles in their own practice and support their palliative care colleagues. Patients and families must advocate for comprehensive care that addresses all their needs. Policymakers must create supportive regulatory and reimbursement environments.
The future of healthcare depends on our collective commitment to supporting those who provide compassionate, comprehensive care during life’s most challenging moments. Palliative care nurses have demonstrated what is possible when clinical expertise is combined with genuine human compassion. Now, it’s up to all of us to ensure they have the support, resources, and recognition they need to continue this vital work.
By caring for those who care, we create a healthcare system that truly serves the needs of all people facing serious illness. We honor the dignity of every patient and family, support the dedicated professionals who serve them, and build a foundation for clinically excellent and deeply human healthcare. This is the legacy we can create together—a healthcare system where no one suffers alone, dignity is preserved, and compassion guides every decision. The time for action is now, and the responsibility belongs to all of us.
Palliative care begins with caring for nurses
Nurses’ experiences of compassionate care in the palliative pathway
Nursing and the Future of Palliative Care
Nursing’s role in leading palliative care: A call to action
Embedding a Palliative Approach in Nursing Care Delivery
End of life care: how nurses can use a compassionate approach
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Clinical Practice Guidelines for Quality Palliative Care, 4th edition
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.
Holistic Nurse: Skills for Excellence book series