Tag: Terminal Disease Progression
Articles about the progression of terminal diseases including how to help provide comfort for terminally ill patients.
Articles about the progression of terminal diseases including how to help provide comfort for terminally ill patients.
Learn the difference between a terminal prognosis and a diagnosis, and get practical tips and resources to help you and your loved one navigate this challenging time.
When a loved one is diagnosed with a terminal illness or a progressive disease, it can be a daunting and overwhelming experience for families and caregivers. Understanding the terms and concepts associated with these conditions is essential to providing the best possible care and support. This article aims to clarify the complex journey of terminal illnesses and progressive diseases, offering guidance and compassion to those navigating this challenging path.

Explore the natural shift in nutritional needs during hospice care. This guide offers insights into managing reduced calorie intake, ensuring comfort and dignity in the end-of-life journey.

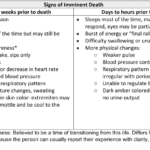
Facing the reality of a loved one's terminal illness can be a challenging and emotional journey. As a hospice registered nurse case manager, I understand the importance of providing compassionate and clear information to empower patients, caregivers, and families. In this article, we'll explore how you, as a family member, can use your own observations and senses to recognize the signs that your loved one may be in the terminal stage of their illness. Remember, while medical professionals have their tools, your observations and intuition significantly matter.
Explore the journey through terminal illness, understanding key signs and symptoms at each stage. This guide offers insight into the physical and emotional changes as life nears its end, helping caregivers provide compassionate support.
Navigating the tender journey of hospice care, Compassion Crossing offers guidance on addressing the pivotal question of “when?”—a beacon for caregivers seeking solace and understanding in life’s final chapter.
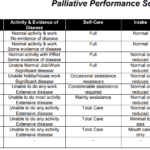
Explore the Palliative Performance Scale (PPS) and its crucial role in end-of-life care. Learn how this tool helps hospice professionals assess patient decline, predict life expectancy, and provide tailored care. Understand the significance of PPS changes in the final six months and how they guide compassionate care decisions.
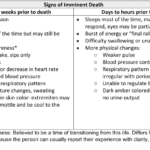
Recognizing end-of-life signs can be challenging. This guide outlines key symptoms indicating a terminally ill patient may have less than two weeks, offering crucial insights for caregivers and families.
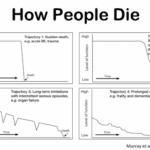
Explore the journey of functional decline in the natural dying process. This article provides insight for caregivers and families, emphasizing the importance of documenting changes to enhance care and decision-making in life’s final chapter.

Hospice nurses assess the status of the patient's journey towards the end of life every nursing visit. Situations where a reversible condition can drastically impact the patient and the hospice assessment can occur. If it is not caught, it is potentially mistreated, leading to increased discomfort and a faster death, often involving increased suffering. One of the common clues that someone is getting closer to dying is increased agitation and restlessness.
Are you aware of Serotonin Syndrome?
Discover key indicators for end-of-life care in hospice. This guide highlights ‘trigger words’ that signal a patient’s final days, aiding nurses and caregivers in providing compassionate support during the most critical moments.
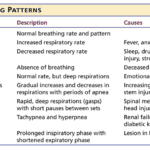
Understanding the final breath: This article explores the critical breathing patterns observed in the last hours of life, offering insights for caregivers and family members to prepare for the end-of-life journey.

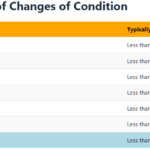
Recognizing the velocity of changes in a patient's condition is crucial for hospice nurses. By understanding the pace of changes in vital signs, symptoms, functionality, and more, nurses can anticipate needs, adjust care plans, and communicate the prognosis effectively with patients and families. The article provides guidelines on interpreting the velocity to estimate the time a patient has left.