Tag: Hospice at a Facility
Articles about hospice services provided at personal care homes, assisted living facilities, memory care, and skilled nursing facilities.
Articles about hospice services provided at personal care homes, assisted living facilities, memory care, and skilled nursing facilities.
This comprehensive guide provides valuable insights on how to report and prevent elderly abuse in nursing homes. It serves as a resource for families, guardians, and loved ones to understand their roles and responsibilities in advocating for the elderly. Learn how to empower yourself and ensure the safety and well-being of your loved ones.

Deciding between home care and facility care for a terminally ill loved one requires careful consideration of medical, emotional, and practical factors to ensure comfort and dignity.

This comprehensive guide empowers families to navigate care plan meetings for terminally ill loved ones. Learn the significance of these meetings, how to prepare, communicate your loved one's needs, and advocate for their best interests. Gain insights into recognizing when meetings are necessary and the benefits of regular care planning. Equip yourself with the knowledge to ensure your loved one receives personalized, dignified care aligned with their wishes.

Explore practical solutions for managing disappearing clothing in dementia care. Learn about iron-on name labels, simplified clothing choices, and the importance of family-facility collaboration. This guide offers practical tips to ensure your loved one with dementia always has the right clothes, reducing stress for patients and caregivers.
Hospice care is often misunderstood. A common myth suggests that once a patient with a terminal illness enters hospice, they lose control over their care. This article aims to dispel this misconception and highlight the central role of patient and family autonomy in hospice settings. It's important to note that this discussion primarily applies to patients receiving care at home or in non-facility settings, as facility-based patients may have less control over their care decisions.
Hospice care in facilities can face challenges due to facility policies, staffing issues, and lack of coordination with hospice providers. This article sheds light on the struggles patients, families, and hospice nurses face in ensuring timely, appropriate care.

Deciding on a dementia care facility is crucial. This guide compares personal care homes, assisted living, memory care units, and nursing facilities, detailing Medicaid eligibility, pros and cons, and essential questions to ensure the best care for your family member.
Uncover the importance of regular care plan meetings at healthcare facilities. This guide details participants, goals, benefits, and risks of non-participation.
When someone you love is extremely sick and needs hospice care, you may feel scared, sad, or angry. You may not know what to do or how to help them. You are not alone. Many people go through this challenging time.
As a hospice nurse, I have met many families who have loved ones in hospice. Some of them are continually active and involved in their care. They ask questions, make decisions, and speak up for their needs. Others are more passive and trusting. They let the doctors, nurses, and staff do whatever they think is best. They don’t say much or ask for anything.
Who do you think gets better care for their loved ones? The active ones or the passive ones?

Caring for a loved one who has a terminal illness can be extremely rewarding but also particularly challenging. You may feel exhausted, overwhelmed, or isolated by the demands of caregiving. You may also feel guilty or anxious about taking a break from your loved one. But you deserve time to rest, recharge, and care for yourself. That is why hospice respite care can be a great option for you and your loved one.
Hospice respite care is a service that allows you to temporarily place your loved one in a facility, such as a hospital, nursing home, or hospice house, where they can receive professional care and support. You can use this time to do whatever you need or want, such as sleeping, working, running errands, visiting friends, or enjoying a hobby. Respite care can last up to five days at a time.

Elopement is when a person with dementia leaves a safe area, like their home or care facility, without supervision. This can be intentional or unintentional, and it's important to address to ensure the safety of the patient. If your loved one is attempting to escape from a memory care facility, there are steps you can take to support both them and the facility.

This article will try to help you cope with this challenge. We will give you some information and advice on how to:
Prepare for the transition to a nursing home
Support your loved one during and after the move
Take care of yourself and your family.

Identifying when a patient may benefit from hospice care is a critical yet often challenging task. For caregivers, including Certified Nursing Assistants (CNAs) and Medical Technicians (Med Techs), visual observation can be a powerful tool for recognizing signs that suggest a hospice referral might be appropriate.
This guide is tailored to assist caregivers in personal care facilities in identifying these signs through visual observation methods, helping provide compassionate and timely end-of-life care.

Memory care admission can be a challenging journey, especially when a family member is grappling with dementia. This transition demands logistical considerations and a deep understanding of the emotional and psychological aspects. As an experienced hospice nurse, I've encountered numerous families navigating this path, and here's a guide to compassionately help your loved one with dementia transition to a memory care unit.

Deciding on end-of-life care for a loved one is challenging and emotional. One major decision to make is whether to opt for home hospice or hospice care at a facility. Both options have advantages and drawbacks, and understanding the pros and cons can help families make an informed choice. Here, we'll explore the pros and cons of each option and provide key questions that families should ask themselves to aid in their decision-making process.

As a family member of a terminally ill loved one receiving care in a facility, you play a vital role in ensuring they receive the best possible care and support during their journey towards a good death. Advocating for your loved one involves understanding their needs, communicating effectively with the facility staff, and staying informed about their care plan. This article aims to guide you on being an effective advocate, asking the right questions, and ensuring your loved one's comfort and well-being.
As an experienced hospice visiting registered nurse, today offered me profound insights from two interconnected perspectives. The first highlights the blind trust we often place in facility nurses and doctors when caring for our loved ones. The second involves the challenges I encountered while advocating for proper end-of-life care for a patient with Alzheimer's.
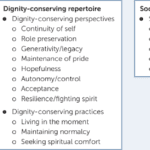
Educating nursing home staff on hospice care priorities like shifting focus from vital signs to comfort, managing symptoms like pain/breathlessness, providing psychosocial support, end-of-life planning, and bereavement care is crucial. Hospice emphasizes quality of life over curative treatments. Effective symptom management through medications and non-pharmacological approaches enhances patient comfort. Open communication, empathy, and respecting patient autonomy are essential. Hospice prepares families for the dying process and grief counseling.

What does a typical day, a typical week look like for a visiting hospice registered nurse case manager look like?

One of the hardest portions of the job of a hospice nurse is to identify when a patient has two weeks of life left to live; this can be especially difficult at facilities going through staffing shortages leading to inconsistent caregivers with little to verbally report on a patient’s change of condition. Since being aware of the velocity of declines is extremely important, let’s cover an area that we in hospice (nurses, families, and caregivers alike) can keep an eye on in terms of identifying terminal restlessness which is often a key indicator for one week or less of life.
Falls among the elderly can have severe consequences, including hip fractures, which can be life-threatening. As an experienced hospice registered nurse case manager, I understand the importance of fall prevention, especially in private homes, personal care homes, and assisted living facilities. This article aims to provide practical tips for reducing falls in these settings by following the nursing process: assessment, diagnosis, planning, implementation, and evaluation.