Tag: Changes in Condition
Articles about changes in condition in the terminally ill often resulting in being closer to death.
Articles about changes in condition in the terminally ill often resulting in being closer to death.

Hospice nurses assess the status of the patient's journey towards the end of life every nursing visit. Situations where a reversible condition can drastically impact the patient and the hospice assessment can occur. If it is not caught, it is potentially mistreated, leading to increased discomfort and a faster death, often involving increased suffering. One of the common clues that someone is getting closer to dying is increased agitation and restlessness.
Are you aware of Serotonin Syndrome?
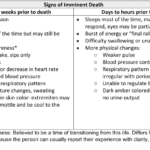
Discover key indicators for end-of-life care in hospice. This guide highlights ‘trigger words’ that signal a patient’s final days, aiding nurses and caregivers in providing compassionate support during the most critical moments.
Caring for a loved one with a history of diverticulitis requires a combination of preventive measures, early detection of warning signs, and understanding the common signs and symptoms of this condition. Your role as a caregiver is crucial in providing support and assistance to ensure their well-being. In this comprehensive guide, we will explore essential aspects of caring for someone with diverticulitis, including prevention, early warning signs, and treatment options.
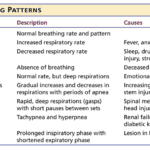
Understanding the final breath: This article explores the critical breathing patterns observed in the last hours of life, offering insights for caregivers and family members to prepare for the end-of-life journey.

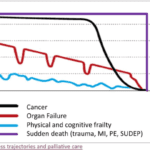
Caring for a terminally ill loved one can be challenging. Still, with the proper support and understanding, you can help ensure they experience a comfortable and dignified end of life. Hospice care offers specialized medical and emotional support during this time. This guide aims to empower families new to hospice services by providing essential information on what to expect from a hospice provider and how to manage the journey towards a good death.

Recognizing the velocity of changes in a patient's condition is crucial for hospice nurses. By understanding the pace of changes in vital signs, symptoms, functionality, and more, nurses can anticipate needs, adjust care plans, and communicate the prognosis effectively with patients and families. The article provides guidelines on interpreting the velocity to estimate the time a patient has left.
When someone you love is sick and may not get better, you want to do everything possible to make them comfortable and happy. Sometimes, you may notice that they are acting differently or feeling worse. This is called a change of condition. Some changes in condition are very serious and need to be reported to the hospice provider right away. Other changes in condition are less urgent and can be written down in a journal until the next nursing visit. This article will help you learn how to tell the difference and what to do.

Caring for a loved one in hospice is rewarding yet challenging. Keeping a caregiver journal benefits the patient, family, and hospice provider. It enhances care, coping, and creating memories. Get tips on starting and maintaining a meaningful journal to improve your caregiving experience.

There are observation and interviewing skills you can develop which will help you learn:
What could cause the current change in condition
Determining if a patient is having terminal restlessness
Determining if your patient is within two weeks or less of life to live
Knowing where your patient is in the dying process
While this article is primarily meant for new nurses, what I’m sharing is also valuable for family members and loved ones. Anyone with patience and love toward the person being observed and interviewed can hone and develop these skills.
As nurses, when we see an acute change of condition, part of what we should be doing in our assessment is determining if there are reversible or treatable elements that are causing the change. In RN school, Dr. Dagen taught the students about using the D.O.G. mnemonic to help us remember that if a patient has an acute change of condition to check whether there were new medications the patient is taking, their O2 saturation level and their glucose level.
I would further add that as a hospice nurse dealing with mainly geriatric patients that if there is an altered level of consciousness (LOC)/personality change, to also consider the patient may have an infection. For any of you dealing with geriatric patients add “I” for infection, hence “D.O.G.I.” While this mnemonic is typically used for acute changes of level of consciousness, the thought process behind it can be used for other acute change of patient condition as well.

The dying process involves physical and emotional changes as the body shuts down. As the heart weakens, circulation slows, leading to cold hands and feet, pale skin, and drowsiness. Breathing becomes irregular and shallow. The patient may experience delirium or visions. Providing comfort through pain management, emotional support, and spiritual care is crucial.

Navigating the final days of a loved one's life can be a challenging and emotional journey. One of the signs that can be observed during this time is known as terminal restlessness. As someone deeply rooted in hospice care, I have witnessed various manifestations of this restlessness. Understanding its types, causes, and management strategies is crucial for providing compassionate end-of-life care. This article aims to illuminate the different kinds of terminal restlessness, identify reversible causes, and discuss effective management techniques. By equipping caregivers, families, and healthcare professionals with this knowledge, we can ensure that terminally ill individuals experience comfort and dignity in their final days.