Understanding respiratory mucus plugs is crucial, especially for those navigating the challenges of caring for terminally ill patients. As an experienced hospice nurse, I recognize the significance of addressing respiratory issues with empathy and clarity. This article aims to provide valuable insights into respiratory mucus plugs, their causes, diagnosis, treatment, prevention, and practical techniques to enhance lung function.
What are Respiratory Mucus Plugs
Mucus is a sticky, slimy substance produced by the cells lining the respiratory tract. Mucus has several important functions in lung health, such as:
- It traps dust, bacteria, viruses, and other foreign particles that enter the airways and prevents them from reaching the lungs.
- Lubricating the airways and reducing friction during breathing.
- Moisturizing the air that reaches the lungs and preventing dehydration.
- Protecting the airways from irritation and inflammation.
Respiratory mucus plugs are clumps or masses of mucus blocking or obstructing the airways, usually the smaller bronchi and bronchioles. Respiratory mucus plugs can affect airflow and oxygen levels in several ways, such as:
- Reducing the amount of air that can enter and exit the lungs.
- Increasing the work of breathing and causing shortness of breath.
- Impairing gas exchange and causing low oxygen levels in the blood.
- Increasing the risk of infection and inflammation in the lungs.
Some examples of symptoms of respiratory mucus plugs are:
- Coughing, sometimes with blood or mucus.
- Wheezing, crackles, or other abnormal breath sounds.
- Chest pain or tightness.
- Difficulty breathing or rapid breathing.
- Bluish color of the skin, lips, or nails (cyanosis).
- Fatigue or weakness.
- Fever or chills.
- Confusion or altered mental status.
What Causes Respiratory Mucus Plugs?
Many medical conditions can cause excessive or thick mucus production, leading to mucus plugs in the airways. Some of the common ones are:
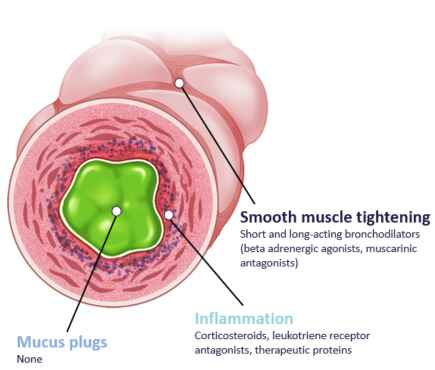
- Asthma: A chronic condition that causes inflammation and narrowing of the airways, making them more sensitive to triggers such as allergens, irritants, or infections. Asthma can cause mucus to build up in the airways, especially during an asthma attack.
- Cystic fibrosis: A genetic disorder that affects the cells that produce mucus, sweat, and digestive juices. Cystic fibrosis causes these fluids to become thick and sticky, clogging the airways and making breathing hard.
- Chronic obstructive pulmonary disease (COPD) is a group of lung diseases that includes chronic bronchitis and emphysema. COPD damages the airways and alveoli, reducing airflow and oxygen levels in the lungs. It also causes increased mucus production and chronic cough.
- Nervous system disorders: Some conditions that affect the brain or spinal cord, such as stroke, multiple sclerosis, or amyotrophic lateral sclerosis (ALS), can impair the ability to cough or swallow. This can result in mucus accumulation in the airways and difficulty clearing it.
Some factors can contribute to mucus plugging, such as:
- Being sedentary: Lack of physical activity can reduce the lung capacity and the effectiveness of coughing. This can make it harder to expel mucus from the airways.
- Weak muscles: Muscle weakness, especially in the chest and abdomen, can affect the ability to breathe deeply and cough forcefully. This can also lead to mucus retention in the airways.
- Impaired vocal cords: Vocal cord dysfunction or paralysis can cause the vocal cords to close or narrow the airway, making breathing difficult or coughing. This can also trap mucus in the airways.
- Dehydration: Not drinking enough fluids can cause the mucus to become thicker and stickier, making it harder to move and clear from the airways.
- Tracheostomy tube: A tracheostomy is a surgical procedure that creates an opening in the neck to insert a tube into the windpipe. This can bypass the upper airway and allow air to enter the lungs directly. However, a tracheostomy tube can also increase the risk of mucus plugging, as it can interfere with the normal mucus clearance mechanisms and cause irritation and inflammation in the airways.
How are Respiratory Mucus Plugs Diagnosed?
Some tests that can help diagnose mucus plugs are:
- Lung function tests: These are a group of tests that measure how well the lungs work by assessing lung volume, capacity, rates of flow, and gas exchange. Lung function tests can detect obstructive or restrictive lung diseases that can cause mucus plugs, such as asthma, COPD, cystic fibrosis, or interstitial lung disease. The most common lung function test is spirometry, which measures how much air one can inhale and exhale and how fast one can do it. Other lung function tests include lung volumes, which measure the air in the lungs after different points of inhalation and exhalation, and diffusing capacity, which measures how easily oxygen enters the bloodstream.
- Chest X-ray: This imaging test uses X-rays to create a picture of the heart, lungs, and bones of the chest. A chest X-ray can reveal the presence of mucus plugs in the airways and other conditions that may be associated with them, such as pneumonia, lung cancer, or fluid in or around the lungs. It can also show the size and shape of the heart and the blood vessels in the chest.
- Arterial blood gas test: This is a blood test that measures the levels of oxygen and carbon dioxide in the blood and its pH balance. It can help evaluate how well the lungs can move oxygen into the blood and remove carbon dioxide from the body. It can also indicate the presence of acid-base disorders that may affect the respiratory system. An arterial blood gas test requires a sample of blood from an artery, usually in the wrist, groin, or elbow.
How are Respiratory Mucus Plugs Treated?
Some medications that can help loosen or thin mucus are:
- Bronchodilators: These drugs relax the muscles around the airways and open them up, making it easier to breathe and cough. They can be taken as inhalers, nebulizers, or pills. Some examples are albuterol, salmeterol, and theophylline.
- Expectorants are drugs that increase the amount of water in mucus, making it thinner and less sticky. They can help clear mucus from the lungs by coughing or suctioning. Expectorants can be taken as syrups, tablets, or capsules. The most common expectorant is guaifenesin, found in products like Robitussin and Mucinex.
- Decongestants are drugs that reduce the swelling and inflammation of the nasal and sinus passages, which can also affect the lower airways. They can help decrease mucus production and congestion. They can be taken as nasal sprays, drops, or pills. Some examples are pseudoephedrine, phenylephrine, and oxymetazoline. However, decongestants should be used with caution, as they can cause side effects such as increased blood pressure, heart rate, and insomnia.
- Mucolytics: These drugs break down the chemical bonds of mucus, making it less thick and sticky. They can help dissolve mucus plugs and improve airflow and oxygen levels. They can be taken as nebulizers, inhalers, or pills. Some examples are N-acetylcysteine, carbocysteine, and dornase alfa.
Some non-pharmacological treatments that can help remove mucus plugs are:
- Chest physiotherapy (CPT) involves applying manual pressure, vibration, or percussion to the chest wall or changing the body position to loosen and mobilize the mucus. A trained therapist, a caregiver, or a device can do CPT. CPT can help improve the cough and clear the airways.
- Cough assist machine: This device applies positive and negative pressure to the airways, mimicking a natural cough. It can help expel mucus from the lungs and prevent mucus plugging. Patients with weak cough muscles or impaired vocal cords can use it.
- Suctioning: This procedure involves inserting a thin tube into the mouth, nose, or tracheostomy tube and applying suction to remove mucus from the airways. Suctioning can help relieve the symptoms of mucus plugging and prevent complications such as infection and atelectasis. It can be done by a healthcare professional, a caregiver, or the patient themselves.
How can Respiratory Mucus Plugs be Prevented?
One of the most important ways to prevent respiratory mucus plugs is to keep the mucus thin and moist. This can be achieved by:
- Drinking enough fluids: Water is the best drink, as it helps hydrate the body and mucus. Other liquids, such as juice, tea, or broth, can also help, but avoid drinks that contain caffeine, alcohol, or sugar, as they can dehydrate the body and mucus.
- Using a humidifier or vaporizer: These devices can add moisture to the air, which can help prevent the mucus from drying out and becoming thick. They can also help soothe the airways and reduce irritation and inflammation. However, clean and maintain the humidifier or vaporizer regularly, as they can harbor bacteria or mold if not used properly.
Another way to prevent respiratory mucus plugs is to improve lung function and mucus clearance. This can be done by:
- Doing breathing exercises: These exercises can help strengthen the respiratory muscles, increase lung capacity, and enhance gas exchange. They can also help loosen and mobilize the mucus, making it easier to cough or suction. Some examples of breathing exercises are pursed-lip, diaphragmatic, and huff coughing.
Breathing Exercises
Pursed-lip Breathing
Pursed-lip breathing is a technique for slowing down and exhaling more air. It can also help you relax and reduce stress.
- Sit or stand with your back straight and your shoulders relaxed.
- Breathe in slowly through your nose, keeping your mouth closed. You can count to two in your head as you inhale.
- Purse your lips as if you will whistle or blow out a candle.
- Breathe out gently through your pursed lips, making a soft hissing sound. You can count to four in your head as you exhale. Try to exhale twice as long as you inhale.
- Repeat this cycle for about 10 minutes or until you feel comfortable.
Diaphragmatic Breathing
Diaphragmatic breathing is a technique that helps you use your diaphragm, the main muscle of breathing, more effectively. It can help you take deeper breaths and increase the oxygen in your blood.
- Lie on your back on a flat surface or a bed, with your knees bent and a pillow under your head. For more support, you can also place a pillow under your knees.
- Place one hand on your upper chest and the other on your abdomen below your rib cage.
- Breathe slowly through your nose, feeling your abdomen rise with your hand. Your chest should remain still or move slightly.
- Breathe slowly through your mouth or nose, feeling your abdomen fall with your hand. You can gently press on your abdomen to help you exhale.
- Repeat this cycle for about 10 minutes or until you feel comfortable.
Huff Coughing
Huffing coughing is a technique for clearing mucus from your lungs and airways. It involves exhaling forcefully through your mouth, making a huffing sound. It can be more effective and less tiring than regular coughing.
- Sit or stand with your back straight and your shoulders relaxed.
- Take a deep breath through your nose, filling your lungs with air. You can hold your breath for a few seconds if you want.
- Open your mouth and exhale quickly and forcefully, making a “ha” or “huff” sound. You should feel your chest and abdomen contract as you exhale.
- Repeat this cycle two or three times, depending on how much mucus you have. You can vary the length and force of your huffs, such as a long breath in and a short huff out or a short breath in and out.
- Follow with a strong cough to clear the mucus from your throat. You can spit out the mucus into a tissue or a cup.
- Repeat this cycle until you feel your lungs and airways are clear.
- Using devices that can help expand the lungs and clear the airways: These devices can help improve lung function and mucus clearance by applying positive pressure, vibration, or oscillation to the airways. They can also help stimulate the cough reflex and expel mucus from the lungs. Some examples of these devices are incentive spirometers, flutter valves, and capsella devices.
Finally, it is important to consult your doctor if you have any concerns or questions about respiratory mucus plugs. Your doctor can help you:
- Identify and treat the underlying cause of mucus plugs: Your doctor can diagnose the condition causing the mucus plugs, such as asthma, cystic fibrosis, COPD, or a nervous system disorder, and prescribe the appropriate medication or therapy to manage it.
- Monitor and adjust your treatment plan: Your doctor can check your lung function, oxygen levels, and mucus quality and adjust your treatment plan accordingly. Your doctor can also recommend the best devices and techniques for mucus clearance and prevention.
- Prevent and treat complications: Your doctor can help you prevent and treat any complications that may arise from mucus plugs, such as infection, inflammation, or atelectasis. Your doctor can also refer you to a specialist or a hospital if needed.
Conclusion
Understanding respiratory mucus plugs is vital for caregivers, families, and healthcare professionals dealing with terminally ill patients. Recognizing symptoms, understanding causes, and implementing preventive measures can enhance the quality of life for those in our care.
Resources
Airway-Occluding Mucus Plugs and Mortality in Patients With Chronic Obstructive Pulmonary Disease
Plugs of the Air Passages
How Do You Get Rid of a Mucus Plug in Your Lungs?
ALS Association Fact Sheet on Mucus Plugs
Thick, Sticky Mucus: Symptoms, Causes, and Treatment
Mucus Dysregulation in COPD and Asthma Causes Mucus Plug Formation and Airway Obstruction
Pursed Lip Breathing: Technique, Purpose & Benefits
Diaphragmatic Breathing Exercises & Benefits
Huff Cough: Huffing, Maneuver, Purpose & How To
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
The National Academy of Elder Law Attorneys (NAELA) is dedicated to improving the quality of legal services provided to older adults and people with disabilities
Articles on Advance Directives
Eldercare Locator: a nationwide service that connects older Americans and their caregivers with trustworthy local support resources
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Caregiver Support Book Series
VSED Support: What Friends and Family Need to Know
My Aging Parent Needs Help!: 7-Step Guide to Caregiving with No Regrets, More Compassion, and Going from Overwhelmed to Organized [Includes Tips for Caregiver Burnout]
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Dear Caregiver, It’s Your Life Too: 71 Self-Care Tips To Manage Stress, Avoid Burnout, And Find Joy Again While Caring For A Loved One
Everything Happens for a Reason: And Other Lies I’ve Loved
The Art of Dying
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying