Introduction
If you are caring for a loved one with pulmonary fibrosis, you may have many questions and concerns about their condition and how to support them best. You may also feel overwhelmed, stressed, or isolated by the challenges and responsibilities of caregiving. You are not alone. Many people face similar situations and emotions when caring for someone with chronic and progressive lung disease.
This article will help you understand pulmonary fibrosis and how it affects your loved one and yourself. It will also provide practical and helpful information on giving the best care for your loved one and yourself. By reading this article, you will learn:
- What pulmonary fibrosis is, and what causes it
- What are the signs and symptoms of pulmonary fibrosis and how they may change over time
- What are the treatment options and management strategies for pulmonary fibrosis
- When and how to involve hospice care for your loved one with pulmonary fibrosis
- How to take care of yourself as a caregiver and cope with the stress and emotions of caregiving
We hope this article will help you gain more knowledge and confidence in your role as a caregiver and make your journey easier and more rewarding. Remember that you are not alone and that many resources and support groups are available for you and your loved one. You are doing a great job; we are here to support you.
What is Pulmonary Fibrosis?
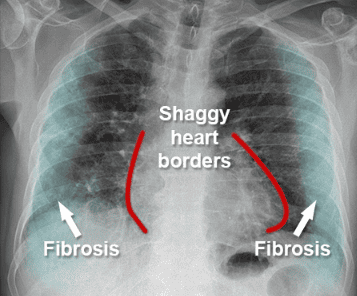
Pulmonary fibrosis is a condition that causes scarring and thickening of the lung tissue. The word “pulmonary” means lung, and the word “fibrosis” means scar tissue. The scar tissue makes it harder for the lungs to work properly and to move oxygen into the blood. Oxygen is a gas that the body needs to function and stay alive.
There are many different types and causes of pulmonary fibrosis. Some types are inherited, which means they are passed down from parents to children. Some types are caused by exposure to harmful substances, such as dust, chemicals, or radiation. Some types are related to other medical conditions, such as autoimmune diseases, infections, or cancer. Some types have no known cause and are called idiopathic pulmonary fibrosis.
Pulmonary fibrosis affects the lungs in different ways. Scar tissue can make the lungs stiffer and less elastic, which means they cannot expand and contract as well as they should. Scar tissue, called alveoli, can also damage the tiny air sacs in the lungs, where oxygen and carbon dioxide are exchanged. Scar tissue can also affect the blood vessels in the lungs, increasing the pressure in the lungs and the heart.
Pulmonary fibrosis is a serious and progressive disease, which means it gets worse over time. It can affect people of any age, but it is more common in older adults. According to the Pulmonary Fibrosis Foundation, about 200,000 people in the United States have pulmonary fibrosis, and about 50,000 new cases are diagnosed each year 1. Pulmonary fibrosis can reduce the life expectancy and quality of life of people with it. It can also lead to complications, such as lung infections, blood clots, lung cancer, heart failure, and respiratory failure.
Some factors can increase the risk of developing pulmonary fibrosis or make it worse. These include:
- Smoking or exposure to secondhand smoke
- Having a family history of pulmonary fibrosis or other lung diseases
- Working or living in environments where you breathe in dust, fumes, or gases, such as asbestos, silica, coal, or metal
- Having certain medical conditions, such as rheumatoid arthritis, scleroderma, sarcoidosis, or gastroesophageal reflux disease (GERD)
- Taking certain medications, such as chemotherapy drugs, antibiotics, or anti-inflammatory drugs
- Having radiation therapy to the chest
If you or a loved one has pulmonary fibrosis, it is important to know the type and cause of the disease, as this can affect treatment and prognosis. It is also important to follow the advice of your doctor or other healthcare professional and seek help if you notice any changes or worsening of your symptoms.
Signs and Symptoms of Pulmonary Fibrosis
Pulmonary fibrosis can cause different signs and symptoms depending on how severe it is and how fast it progresses. Some of the most common ones are:
- Shortness of breath. This is the main symptom of pulmonary fibrosis. It means having difficulty breathing or feeling out of breath, especially during physical activity or exertion. Shortness of breath can also occur at rest or when lying down. It can make you feel anxious, tired, or frustrated. It can also limit your ability to do things you enjoy or need to do, such as walking, climbing stairs, or working.
- Dry cough. This is another common symptom of pulmonary fibrosis. It means having a persistent or chronic cough that produces no mucus or phlegm. A dry cough can be irritating, painful, or annoying. It can also interfere with your sleep, appetite, or speech. It can also make you feel embarrassed or self-conscious in social situations.
- Fatigue means feeling exhausted, even after resting or sleeping. It can be caused by low oxygen levels in the blood, poor sleep quality, or the extra effort required to breathe. Fatigue can affect your mood, concentration, memory, or motivation. It can also make you feel weak, dizzy, or faint.
- Unexplained weight loss. This means losing weight without trying or without a clear reason. Weight loss can be caused by loss of appetite, difficulty swallowing, or increased metabolism due to the extra work of breathing. Weight loss can also lead to muscle mass, strength, or bone density loss. It can also make you more prone to infections or complications.
- Aching muscles and joints. This means having pain, stiffness, or inflammation in your muscles or joints, especially in the chest, back, or shoulders. The strain of breathing, coughing, or posture changes can cause aching muscles and joints. They can also be related to other conditions, such as arthritis, that may occur along with pulmonary fibrosis. Aching muscles and joints can make moving, exercising, or relaxing harder.
- Widening and rounding of the tips of the fingers or toes, also known as clubbing, means changes in the shape or appearance of your fingers or toes, such as increased curvature, swelling, or redness. Clubbing can be caused by low oxygen levels in the blood, which can affect the growth of the tissues under the nails. Clubbing can also indicate more advanced or severe pulmonary fibrosis.
These signs and symptoms may vary from person to person and over time. Some people may have more or fewer symptoms than others. Some people may have mild or moderate symptoms for a long time, while others may have severe or worsening symptoms quickly. Some people may have periods of stability or improvement, while others may have periods of exacerbation or deterioration.
These signs and symptoms can affect the quality of life and daily activities of the person with pulmonary fibrosis. They can make breathing, eating, sleeping, working, or enjoying hobbies harder. They can also cause emotional distress, such as anxiety, depression, anger, or fear. They can also affect the relationships, roles, and responsibilities of the person with pulmonary fibrosis and their family, friends, or caregivers.
Here are some examples and scenarios of how these signs and symptoms may manifest:
- John is a 65-year-old retired teacher who was diagnosed with pulmonary fibrosis two years ago. He used to enjoy gardening, hiking, and traveling with his wife, but now he gets short of breath and tired easily. He must use supplemental oxygen when walking or doing any physical activity. He also has a dry cough that keeps him awake at night. He has lost 10 pounds in the last six months and feels weak. He worries about his future and his ability to care for himself and his wife.
- Mary is a 50-year-old nurse who was diagnosed with pulmonary fibrosis six months ago. She has a family history of the disease and was exposed to asbestos at her workplace. She has mild symptoms, such as occasional shortness of breath and dry cough. She still works part-time and tries to stay active and positive. She takes medication to slow down the progression of the disease and attends a pulmonary rehabilitation program to improve her lung function and fitness. She also joins a support group to share her experiences and learn from others with pulmonary fibrosis.
- David is a 40-year-old engineer who was diagnosed with pulmonary fibrosis three months ago. He has no known risk factors or causes for the disease. He has severe symptoms, such as constant shortness of breath, dry cough, fatigue, and weight loss. He must always use high-flow oxygen and has difficulty doing simple tasks, such as dressing, bathing, or eating. He has been hospitalized several times for lung infections and blood clots. He is considering a lung transplant as his last option. He is depressed and isolated and feels like a burden to his family and friends.
How to Provide the Best Care for Loved Ones with Pulmonary Fibrosis
Caring for a loved one with pulmonary fibrosis can be challenging but also rewarding. You can positively impact their lives by providing physical, emotional, and practical support. Here are some goals and principles of care for pulmonary fibrosis:
- Help your loved one maintain their lung function and overall health. This means encouraging them to follow their treatment plan, take their medications, use their oxygen therapy, and avoid smoking and other lung irritants. It also means helping them eat a balanced diet, drink enough fluids, and get enough rest and sleep.
- Help your loved one stay active and independent. This means encouraging them to do physical activities that they enjoy and can safely perform, such as walking, gardening, or yoga. It also means helping them with daily tasks that they may find difficult, such as dressing, bathing, or cooking, but also respecting their preferences and choices.
- Help your loved one cope with their symptoms and emotions. This means listening, validating their feelings, and offering comfort and reassurance. It also means helping them manage their symptoms, such as shortness of breath, cough, fatigue, and pain, using relaxation techniques, distraction methods, or medication.
- Help your loved one plan for the future and make informed decisions. This means discussing their goals, values, and preferences for their care and respecting their wishes. It also means helping them prepare for possible changes or complications, such as worsening symptoms, hospitalizations, or hospice care, by having advance directives, legal documents, and emergency contacts.
One of the most important things you can do as a caregiver is to ensure your loved one has regular medical check-ups and follow-ups. This can help monitor their condition, adjust their treatment, and prevent or treat any complications. You can help your loved one by:
- Keeping track of their appointments and tests. You can use a calendar, a notebook, or an app to record when and where they need to see their doctor or other healthcare professional and what tests they need to do. You can also remind them of their appointments and help them get there.
- Accompanying them to their appointments and tests. You can provide them with company, support, and transportation. You can also help them communicate with their doctor or healthcare professional by asking questions, taking notes, or clarifying information. You can also help them follow their doctor’s instructions and advice.
- Being aware of any changes or concerns. You can observe your loved one’s symptoms, behavior, and mood and report any changes or concerns to their doctor or healthcare professional. You can also watch for any signs of infection, such as fever, chills, or cough, and seek medical attention if needed.
There is no cure for pulmonary fibrosis, but there are some treatment options that can help slow down the progression of the disease, relieve symptoms, and improve quality of life. The treatment options may vary depending on the type and cause of pulmonary fibrosis, the severity of the disease, and the individual’s preferences and goals. Some of the common treatment options are:
- Medications. Pirfenidone and nintedanib are two FDA-approved medications for idiopathic pulmonary fibrosis, the most common type of pulmonary fibrosis. They work by reducing the inflammation and scarring in the lungs. They can help slow down the decline in lung function and prolong survival. However, they also have some side effects, such as nausea, diarrhea, rash, or liver problems. They may not work for everyone or may stop working over time.
- Oxygen therapy is a treatment that provides extra oxygen to the lungs through a nasal cannula, a mask, or a tube. It can help improve blood oxygen levels, reduce shortness of breath, and increase exercise capacity. It can also prevent or treat complications, such as pulmonary hypertension or heart failure. However, oxygen therapy also has challenges, such as finding the right equipment, adjusting the flow rate, and dealing with the stigma or inconvenience.
- Pulmonary rehabilitation is a program that combines exercise, education, and counseling to help people with lung diseases improve their physical and mental health. It can help increase lung function, muscle strength, and endurance. It can also help reduce symptoms such as shortness of breath, fatigue, and anxiety. It can also help improve quality of life, self-confidence, and coping skills. However, pulmonary rehabilitation requires commitment, motivation, and access to a qualified team and facility.
- Lung transplant. This surgery replaces one or both diseased lungs with healthy lungs from a donor. A lung transplant can improve lung function, symptoms, and survival. It can also improve the quality of life and allow for more activities. However, lung transplant also has many risks and challenges, such as finding a suitable donor, waiting for a long time, undergoing a major operation, taking lifelong anti-rejection drugs, and facing possible complications, such as infection, rejection, or cancer.
The decision to start, stop, or change any treatment option should be made in consultation with your loved one’s doctor or other healthcare professional based on their condition, preferences, and goals. You can help your loved one by:
- Learning about the treatment options and their benefits and risks. You can research, read, or watch reliable sources of information, such as the Pulmonary Fibrosis Foundation, the American Lung Association, or the Mayo Clinic. You can also ask your loved one’s doctor or other healthcare professional for more details or clarification.
- Supporting your loved one’s choice and adherence. You can respect your loved one’s decision and help them follow their treatment plan. You can also help them cope with any side effects or difficulties they may experience. You can also encourage them to seek a second opinion or explore other options if they are not satisfied or comfortable with their current treatment.
- Evaluating the effectiveness and outcomes of the treatment. You can monitor your loved one’s response and progress with their treatment. You can also help them keep track of their symptoms, lung function, and quality of life. You can also help them communicate their feedback and concerns to their doctor or healthcare professional and adjust their treatment if needed.
Managing the symptoms and complications of pulmonary fibrosis can be challenging, but there are some strategies and tips that can help you and your loved one. Here are some examples:
- For shortness of breath. You can help your loved one use their oxygen therapy correctly and consistently. You can also help them practice pursed-lip or diaphragmatic breathing exercises to improve their oxygen intake and carbon dioxide removal. You can also help them conserve energy and pace their activities by planning, taking breaks, and using assistive devices.
- For dry cough. You can help your loved one stay hydrated and moisten their throat by drinking water, sucking on ice chips, or using a humidifier. You can also help them avoid irritants and allergens, such as smoke, dust, or perfume, that may trigger or worsen their cough. You can also help them use cough suppressants, expectorants, or lozenges, as prescribed or recommended by their doctor or other healthcare professional.
- For fatigue. You can help your loved one get enough rest and sleep by creating a comfortable and quiet environment, following a regular schedule, and avoiding caffeine, alcohol, or nicotine. You can also help them eat a balanced and nutritious diet by choosing foods high in protein, fiber, and antioxidants and avoiding foods high in fat, sugar, or salt. You can also help them do moderate and low-impact exercises, such as walking, swimming, or cycling, to boost their energy and mood.
- For weight loss. You can help your loved one increase their calorie and protein intake by offering them small and frequent meals and snacks, adding sauces, dressings, or cheese to their foods, and using supplements, shakes, or bars, as advised by their doctor or other healthcare professional. You can also help them improve their appetite and digestion by making mealtime pleasant, avoiding foods that cause gas or reflux, and using medications, such as appetite stimulants or antacids, as prescribed or recommended by their doctor or other healthcare professional.
- For aching muscles and joints. You can help your loved one relieve their pain and inflammation by applying heat or cold packs, massaging or stretching their muscles, or using painkillers, anti-inflammatories, or creams as prescribed or recommended by their doctor or other healthcare professional. You can also help them prevent or reduce their muscle and joint problems by encouraging them to maintain good posture, use ergonomic furniture and equipment, and avoid lifting heavy objects.
- For clubbing, you can help your loved one cope with the changes in their fingers or toes by providing them with emotional support and reassurance. You can also help them care for their nails by keeping them clean, trimmed, and moisturized. You can also help them protect their fingers or toes from injury or infection by wearing gloves, socks, or shoes and avoiding exposure to cold or heat.
These strategies and tips can help you and your loved one manage the symptoms and complications of pulmonary fibrosis. However, depending on your situation and preferences, you may find other ways that work better for you and your loved one. You can consult your loved one’s doctor or other healthcare professional for more guidance and advice.
As a caregiver, you may also benefit from seeking support and information from other sources, such as:
- The Pulmonary Fibrosis Foundation is a national organization that provides education, advocacy, and research on pulmonary fibrosis. It offers various resources and services, such as a patient communication center, a patient registry, a clinical trial finder, a care center network, and a peer support program.
- The American Lung Association is a national organization that works to improve lung health and prevent lung disease. It offers a range of resources and programs, such as a lung helpline, a lung health library, a lung force initiative, a better breathers club, and a living with lung disease support community.
- The Mayo Clinic is a leading medical institution that provides expert care and research for pulmonary fibrosis and other lung diseases. It offers comprehensive and personalized treatment options and educational and supportive resources, such as a pulmonary fibrosis newsletter, podcast, and blog.
These are some of the resources and support groups that can help you and your loved one with pulmonary fibrosis. However, you may find other sources that suit your needs and interests, such as local hospitals, clinics, or organizations. You can also ask your loved one’s doctor or other healthcare professional for more recommendations.
When to Involve Hospice Care for Loved Ones with Pulmonary Fibrosis
Hospice care is a type of care that focuses on providing comfort, dignity, and quality of life for people with terminal illnesses and their families. Hospice care is not a place but a service that can be delivered in different settings, such as a home, hospital, nursing home, or hospice center. Hospice care involves a team of professionals and volunteers who offer medical, emotional, spiritual, and practical support to the patient and the caregiver. Hospice care also includes bereavement support for the family after the patient’s death.
Hospice care may be an option for your loved one with pulmonary fibrosis when their condition becomes advanced and their life expectancy is six months or less. The decision to start hospice care should be based on the patient’s wishes, the doctor’s recommendation, and the family’s agreement. Some of the criteria and indicators for hospice eligibility and referral for pulmonary fibrosis are:
- The patient has severe lung function impairment, such as a forced vital capacity (FVC) of less than 50% or a diffusing capacity of the lung for carbon monoxide (DLCO) of less than 40%.
- The patient has frequent or severe exacerbations or complications, such as respiratory infections, pulmonary hypertension, heart failure, or respiratory failure.
- The patient has significant weight loss, muscle wasting, or malnutrition.
- The patient responds poorly or is intolerant to medical treatments such as medications, oxygen therapy, or pulmonary rehabilitation.
- The patient is highly dependent on others for daily activities such as bathing, dressing, and eating.
- The patient is in high distress or suffering from symptoms such as shortness of breath, cough, fatigue, or pain.
- The patient has a preference for comfort care over aggressive or curative care.
Hospice care can offer many benefits for your loved one with pulmonary fibrosis and you as a caregiver. Some of the benefits are:
- Hospice care can help relieve your loved one’s symptoms and improve their comfort and well-being. Hospice care can provide medications, therapies, equipment, and supplies to manage shortness of breath, cough, pain, and other symptoms. Hospice care can also offer emotional and spiritual support to help your loved one cope with their feelings and beliefs.
- Hospice care can help reduce your loved one’s need for hospitalizations and emergency visits. Hospice care can provide 24/7 access to hospice nurses and doctors who can monitor your loved one’s condition, adjust their treatment, and prevent or treat any complications. Hospice care can also provide respite care, which means temporary relief for you as a caregiver by caring for your loved one for a few hours or days.
- Hospice care can help you respect your loved one’s wishes and values. Hospice care can honor your loved one’s preferences and choices for their end-of-life care, such as where they want to die, who they want to be with, and what they want to happen after their death. Hospice care can also help your loved one achieve their goals and complete their unfinished business, such as saying goodbye, expressing gratitude, or making amends.
- Hospice care can help support you and your family as caregivers. Hospice care can provide education, guidance, and assistance to help you care for your loved one and yourself. Hospice care can also provide counseling, support groups, and bereavement services to help you and your family deal with the stress, grief, and loss of your loved one.
Some common myths and misconceptions about hospice care may prevent or delay your loved one with pulmonary fibrosis and you as a caregiver from considering or accessing hospice care. Some of these myths and misconceptions are:
- Hospice care does not mean giving up hope or hastening death. It means shifting the hope from curing the disease to improving the quality of life. Hospice care does not cause or speed up death. Hospice care respects the natural course of the disease and the patient’s wishes.
- Hospice care is not only for the last days or hours of life. It can be started when the patient has a life expectancy of six months or less. Hospice care can provide more benefits and comfort if it is started earlier rather than later. Hospice care can also be stopped or resumed if the patient’s condition changes or improves.
- Hospice care is not only for cancer patients. It is for any patient with a terminal illness, such as pulmonary fibrosis, heart disease, kidney disease, or dementia. Hospice care can provide specialized and individualized care for different types and stages of diseases.
- Hospice care does not diminish the patient’s control and dignity; it gives the patient more control and dignity. Hospice care allows patients to make decisions and choices about their end-of-life care and helps patients maintain their physical, emotional, and spiritual well-being.
Making the decision and preparing for hospice care can be challenging and complex for your loved one with pulmonary fibrosis and you as a caregiver. Here are some guidance and advice on how to make the decision and prepare for hospice care:
- Talk to your loved one’s doctor or other healthcare professional. They can provide accurate and updated information about your loved one’s condition, prognosis, and treatment options. They can also help you assess your loved one’s eligibility and readiness for hospice care. They can also help you find and contact a hospice provider that meets your loved one’s needs and preferences.
- Talk to your loved one and your family. They can provide you with emotional and practical support and input. They can also help you understand and respect your loved one’s wishes and values for their end-of-life care. They can also help you cope with your feelings and concerns about hospice care and end-of-life care.
- Talk to a hospice representative or counselor. They can provide you with more information and education about hospice care and what it entails. They can also help you address any myths or misconceptions about hospice care. They can also help you complete the necessary paperwork and arrangements for hospice care.
- Talk to yourself. You can also provide yourself with self-care and compassion. You can also help yourself acknowledge and accept your loved one’s condition and situation. You can also help yourself prepare for the changes and challenges that hospice care and end-of-life care may bring. You can also help yourself seek and accept help from others when you need it.
Care for the Caregivers
As a caregiver for a loved one with pulmonary fibrosis, you may face many physical, emotional, and mental challenges. You may have to deal with the daily demands of caregiving, such as providing medical, personal, and practical care, as well as the long-term impact of caregiving, such as coping with the progression of the disease, the uncertainty of the future, and the grief of losing your loved one. You may also have to balance your caregiving role with other roles and responsibilities, such as work, family, or hobbies.
Caregiving can take a toll on your health and well-being. You may experience some signs and symptoms of caregiver stress and burnout, such as:
- Feeling overwhelmed, exhausted, or frustrated
- Having trouble sleeping, eating, or concentrating
- Feeling isolated, lonely, or depressed
- Getting sick more often or having chronic health problems
- Losing interest or enjoyment in things you used to do
- Feeling guilty, angry, or resentful
- Having conflicts or problems with your loved one, family, or friends
Caregiver stress and burnout can affect your ability to care for your loved one and yourself. That is why it is important to practice self-care and coping skills as a caregiver. Self-care and coping skills can help you reduce stress, improve your mood, and enhance your quality of life. Some ways to practice self-care and coping skills are:
- Take care of your physical health. This means eating a balanced diet, drinking enough water, getting enough sleep, and exercising regularly. It also means seeing your doctor for regular check-ups, taking your medications, and managing any health conditions you may have.
- Take care of your emotional health. This means expressing your feelings, seeking support, and finding joy. It also means doing things that relax you, such as meditation, yoga, or breathing exercises. It also means doing things that make you happy, such as reading, listening to music, or watching a movie.
- Take care of your mental health. This means learning about pulmonary fibrosis and caregiving, seeking help, and setting realistic goals and expectations. It also means staying positive, optimistic, and hopeful. It also means challenging negative thoughts, beliefs, or behaviors that may affect your well-being.
- Take care of your social health. This means staying connected, involved, and engaged with your family, friends, and community. It also means asking for and accepting help from others, such as other caregivers, professionals, or organizations. It also means joining a support group, either online or in person, where you can share your experiences and learn from others in similar situations.
You may also need to maintain your social and personal life as a caregiver. This means keeping in touch with your loved ones and friends and spending quality time with them. It also means pursuing your interests and hobbies and doing things that give you a sense of purpose and fulfillment. It also means taking breaks and time off from caregiving and doing something for yourself.
Caregiving for a loved one with pulmonary fibrosis can be hard but also rewarding. You can make a positive difference in their life and yours by providing them with the best care possible and taking care of yourself. Remember that you are not alone and that many resources and support groups are available for you and your loved one. You are doing a great job; we are here to support you.
Conclusion
In this article, we have discussed pulmonary fibrosis and how it affects your loved one and yourself. We have also provided practical and helpful information on giving the best care for your loved one and yourself. Here are some of the main points and key messages of the article:
- Pulmonary fibrosis is a condition that causes scarring and thickening of the lung tissue, making it harder for the lungs to work properly and to move oxygen into the blood.
- Pulmonary fibrosis can cause different signs and symptoms, such as shortness of breath, dry cough, fatigue, weight loss, aching muscles and joints, and clubbing of the fingers or toes. These signs and symptoms can vary from person to person and over time, affecting the quality of life and daily activities of the person with pulmonary fibrosis and their caregiver.
- Pulmonary fibrosis is a severe and progressive disease, which means it gets worse over time and can reduce the life expectancy and quality of life of the person who has it. It can also lead to complications, such as lung infections, blood clots, lung cancer, heart failure, and respiratory failure.
- Pulmonary fibrosis has many different types and causes, and treatment options may vary depending on the type and cause, the severity of the disease, and the individual’s preferences and goals. Some of the common treatment options are medications, oxygen therapy, pulmonary rehabilitation, and lung transplant.
- Hospice care is a type of care that focuses on providing comfort, dignity, and quality of life for people with terminal illnesses and their families. Hospice care may be an option for your loved one with pulmonary fibrosis when their condition becomes advanced and their life expectancy is six months or less. Hospice care can offer many benefits but also pose some challenges for your loved one with pulmonary fibrosis and you as a caregiver.
- Caregiving for a loved one with pulmonary fibrosis can be challenging but also rewarding. You can make a positive difference in their life and yours by providing them with physical, emotional, and practical support. You can also practice self-care and coping skills to reduce stress, improve your mood, and enhance your quality of life. You can also maintain your social and personal life by staying connected, involved, and engaged with your family, friends, and community.
The purpose and scope of this article were to help you understand pulmonary fibrosis and how to support your loved one and yourself best. We hope this article has helped you gain more knowledge and confidence in your role as a caregiver and made your journey easier and more rewarding.
Here are some take-home tips and recommendations for you as a caregiver:
- Learn as much as you can about pulmonary fibrosis and caregiving, and seek reliable and updated information and education sources, such as the Pulmonary Fibrosis Foundation, the American Lung Association, or the Mayo Clinic.
- Communicate openly and honestly with your loved one, family, friends, and healthcare team, and express your feelings, needs, and concerns. Listen to and respect your loved one’s wishes and values for their end-of-life care.
- Seek and accept help from others, such as other caregivers, professionals, or organizations, and do not hesitate to ask for or offer assistance. Join a support group, either online or in person, where you can share your experiences and learn from others in similar situations.
- Take care of your health and well-being, and practice self-care and coping skills, such as eating, sleeping, exercising, relaxing, meditating, or doing things that make you happy. Seek help if you experience any signs or symptoms of caregiver stress or burnout, such as feeling overwhelmed, exhausted, or depressed.
- Balance your caregiving role with your other roles and responsibilities, and take breaks and time off from caregiving when you need it. Pursue your interests and hobbies, and do things that give you a sense of purpose and fulfillment. Maintain your social and personal life, and keep in touch with your loved ones and friends.
You are not alone in this journey. You are doing a great job; we are here to support you. Remember that you are valuable and important and deserve respect, appreciation, and gratitude for your caregiving. Thank you for your dedication and compassion. We wish you and your loved one all the best.
Resources
The Pulmonary Fibrosis Foundation
The American Lung Association
End of life with pulmonary fibrosis | Action for Pulmonary Fibrosis
How to Support Your Loved One with Pulmonary Fibrosis
7 Things Everyone Should Know about Pulmonary Fibrosis
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
The National Academy of Elder Law Attorneys (NAELA) is dedicated to improving the quality of legal services provided to older adults and people with disabilities
Articles on Advance Directives
Eldercare Locator: a nationwide service that connects older Americans and their caregivers with trustworthy local support resources
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Caregiver Support Book Series
VSED Support: What Friends and Family Need to Know
My Aging Parent Needs Help!: 7-Step Guide to Caregiving with No Regrets, More Compassion, and Going from Overwhelmed to Organized [Includes Tips for Caregiver Burnout]
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Dear Caregiver, It’s Your Life Too: 71 Self-Care Tips To Manage Stress, Avoid Burnout, And Find Joy Again While Caring For A Loved One
Everything Happens for a Reason: And Other Lies I’ve Loved
The Art of Dying
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying