The Dying Process at the End of Life
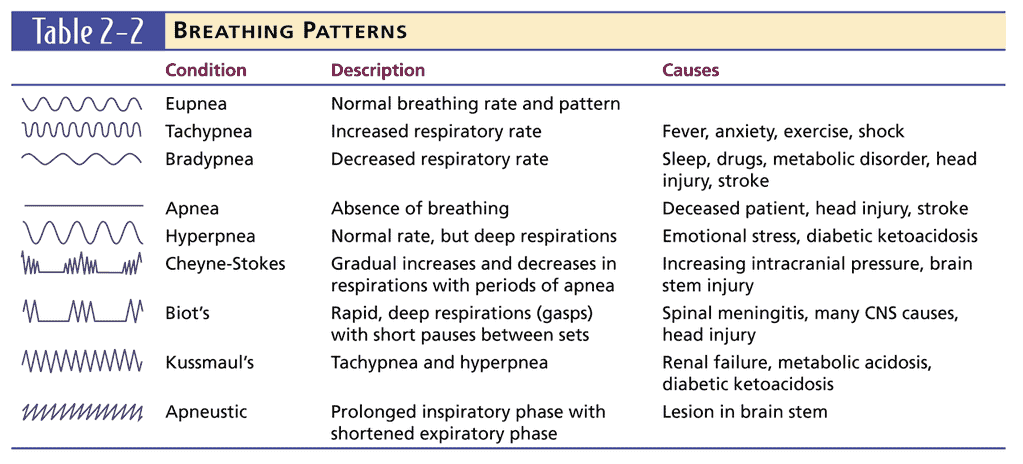
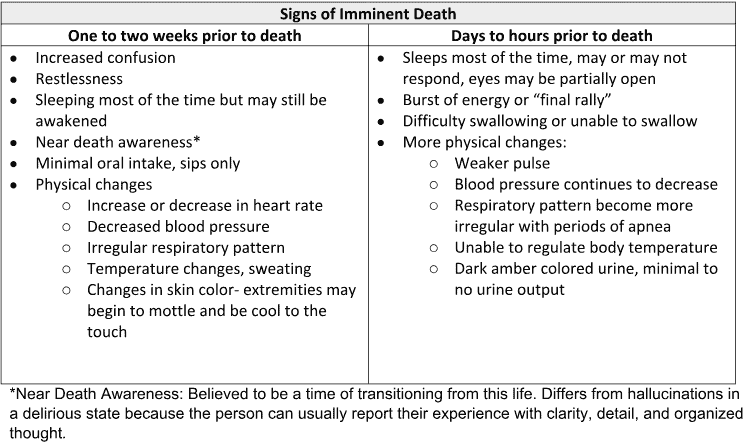
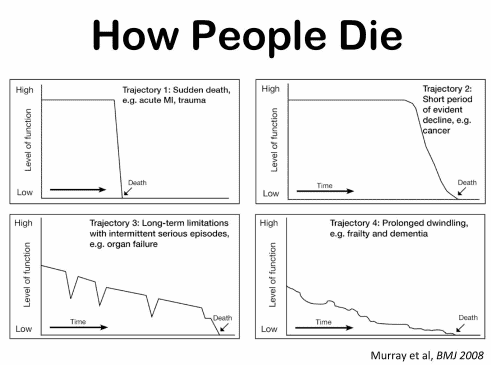
The dying process involves physical and emotional changes as the body shuts down. As the heart weakens, circulation slows, leading to cold hands and feet, pale skin, and drowsiness. Breathing becomes irregular and shallow. The patient may experience delirium or visions. Providing comfort through pain management, emotional support, and spiritual care is crucial.
-

Sleeping as a Prognostication Tool for the Terminally Ill
Sleep patterns can help estimate how close a terminally ill person is to dying. Learn how changes in sleep can indicate approaching death and how to support your loved one during this time. -
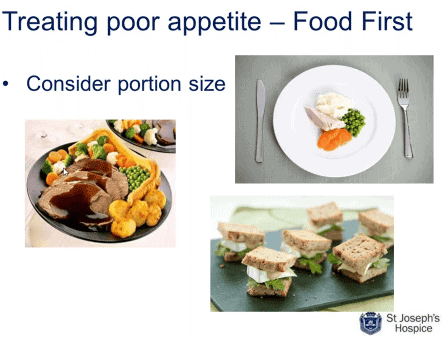
Understanding Nutrition Changes in Hospice: Nourishing Comfort and Peaceful End-of-Life Journey
Explore the natural shift in nutritional needs during hospice care. This guide offers insights into managing reduced calorie intake, ensuring comfort and dignity in the end-of-life journey. -

Understanding the Patient’s Question: When Will I Die?
Navigating the tender journey of hospice care, Compassion Crossing offers guidance on addressing the pivotal question of “when?”—a beacon for caregivers seeking solace and understanding in life’s final chapter.