Explaining Vital Signs to Patients and Families on Hospice
Published on July 29, 2021
Updated on May 21, 2024
Published on July 29, 2021
Updated on May 21, 2024
I don’t know about you, but every time I see a patient and their family for the first time and take their vitals as part of the nursing assessment, either after each vital or at the end of the vital checks, I’m asked something to the effect of “is that good?”
As you, my friendly readers, bloom as hospice nurses, you will learn that the vital sign portion of the assessment is just a smidge of the entire assessment as to whether someone is approaching the end of life, going through reversible or terminal restlessness, or just having a difficult day. Let me share how I educate families that get hyper-focused on vitals.
The education process starts the first time I’m with the patient and family (whether my patient or that of another nurse). Then it is reinforced whenever the patient or family starts getting hypervigilant about vital signs. The framework of what I share is as follows:
We will get vital signs every time I or another nurse visits your loved one. Then I pause and ask them if they have ever been to a museum or an art gallery, somewhere with portraits and pictures where you stand about 6 to 10 feet back… most people have, and if not, then hope for a painting in the room or house you are in. I share, “Vital signs are like the artist’s signature on a painting.” You don’t see them 6 to 10 feet away. You must get up close to see them.” Their size about the painting is relative to their importance. It’s not that the artist doesn’t matter, but the focus is on the painting or picture, not the artist. The same goes for vital signs. Trends may matter over time, but day-to-day until the end of life, the numbers are meaningless. If I see a vital sign of concern due to a trend or moment of crisis, I will alert the doctor and let you know so we can talk about options, but for now, don’t fret about the numbers.
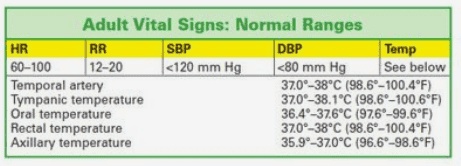
For those of you who are new hospice nurses, know there’s always fine print. Let me go over those vitals that may have meaning based on what you’ve been seeing with the patient:
Various articles with tips for hospice nurses
Teaching the Family What to Expect When the Patient is Dying
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death