Category: Nurse Skills
Articles involving nursing skills and techniques.
Articles involving nursing skills and techniques.
As nurses, when we see an acute change of condition, part of what we should be doing in our assessment is determining if there are reversible or treatable elements that are causing the change. In RN school, Dr. Dagen taught the students about using the D.O.G. mnemonic to help us remember that if a patient has an acute change of condition to check whether there were new medications the patient is taking, their O2 saturation level and their glucose level.
I would further add that as a hospice nurse dealing with mainly geriatric patients that if there is an altered level of consciousness (LOC)/personality change, to also consider the patient may have an infection. For any of you dealing with geriatric patients add “I” for infection, hence “D.O.G.I.” While this mnemonic is typically used for acute changes of level of consciousness, the thought process behind it can be used for other acute change of patient condition as well.
One of the hardest lessons to learn as a nurse, in my experience and opinion, is the psychosocial skills necessary to help patients and their families work towards their healthcare goals. These skills are applicable to every field. While I, myself, am still growing as a registered nurse (heading towards my 5th year at the time of writing this article), I would like to share with you some of the lessons learned. These lessons are based on real-life cases where I will present the scenario, what I did that worked, and what I internally thought of opposite scenarios.
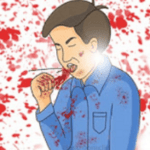
Hemoptysis, or coughing up blood, can be a distressing symptom for patients at the end of their life journey. As a hospice nurse, your expertise in managing this symptom is crucial in ensuring a peaceful and comfortable experience for your patients and their families.

Pain is a subjective sensation that can affect a person’s physical, emotional, and spiritual well-being. While pain can be measured objectively by using vital signs such as temperature, pulse, blood pressure, and respiration count, these indicators may not reflect the true intensity of pain that a person is experiencing. This is especially true for non-verbal patients, who cannot communicate their pain verbally. Non-verbal patients may include those with advanced dementia, terminal illness, or other conditions that impair their speech. In this article, I will discuss the importance of assessing pain in non-verbal patients, the tools and methods that can be used to do so, and the benefits of providing adequate pain relief for these patients.

Navigating the final days of a loved one's life can be a challenging and emotional journey. One of the signs that can be observed during this time is known as terminal restlessness. As someone deeply rooted in hospice care, I have witnessed various manifestations of this restlessness. Understanding its types, causes, and management strategies is crucial for providing compassionate end-of-life care. This article aims to illuminate the different kinds of terminal restlessness, identify reversible causes, and discuss effective management techniques. By equipping caregivers, families, and healthcare professionals with this knowledge, we can ensure that terminally ill individuals experience comfort and dignity in their final days.

One of the main challenges of new nurses is time management. In a hospital or nursing home setting, you often have coworkers to rescue you in a pinch in case you are overwhelmed; on top of having nearby coworkers, most orientation programs, as well as nursing schools, focus on time management skills in a facility setting. Yet what about time management as a visiting nurse — in home health or home hospice or both?
Let me share with you my wisdom and experience in time management in the field of a visiting nurses to hopefully help you have more time for life compared to work — a better work-life balance.

If you are a new nurse to hospice, one of the tasks you probably dread is doing an admission especially if you have scheduled visits the same day as the admission.
I would like to share with you some tips that when applied may help lower your stress level, and help you remain on time even in cases where you have three to four visits including recertification to do the same day.

These are my experiences as a registered nurse caring for geriatric patients in a long-term & rehab care setting where I was the house supervisor responsible for up to 151 residents along with managing the second shift healthcare staff.
By now, you’ve probably had your temperature checked ad nauseam as you visit different locations. Yet, is checking the temperature of your elderly loved ones a good way to know if they may have COVID-19? Are you aware that according to Vital Signs in Older Patients: Age-Related Changes, “older patients are less able to mount a fever response.” Most of my geriatric patients did not have a fever when they contracted COVID-19, and most remained afebrile (without fever) through their stay in the COVID unit.
What’s a more reliable sign of potential COVID-19 infection in the elderly?

As an INFJ, I’m almost constantly introspective. Today, I was helping with an emergency where one of our wonderful on-call nurses was in a car accident. During my visit with a patient I admitted yesterday who is transitioning towards actively dying, I was in bewilderment in my mind about how comfortable and peacefully patient I am when I’m around the terminally ill and their family.