Achieving HCI Excellence: The Ten Moments That Matter Most in Hospice Care
Published on July 21, 2025
Updated on July 18, 2025
Published on July 21, 2025
Updated on July 18, 2025
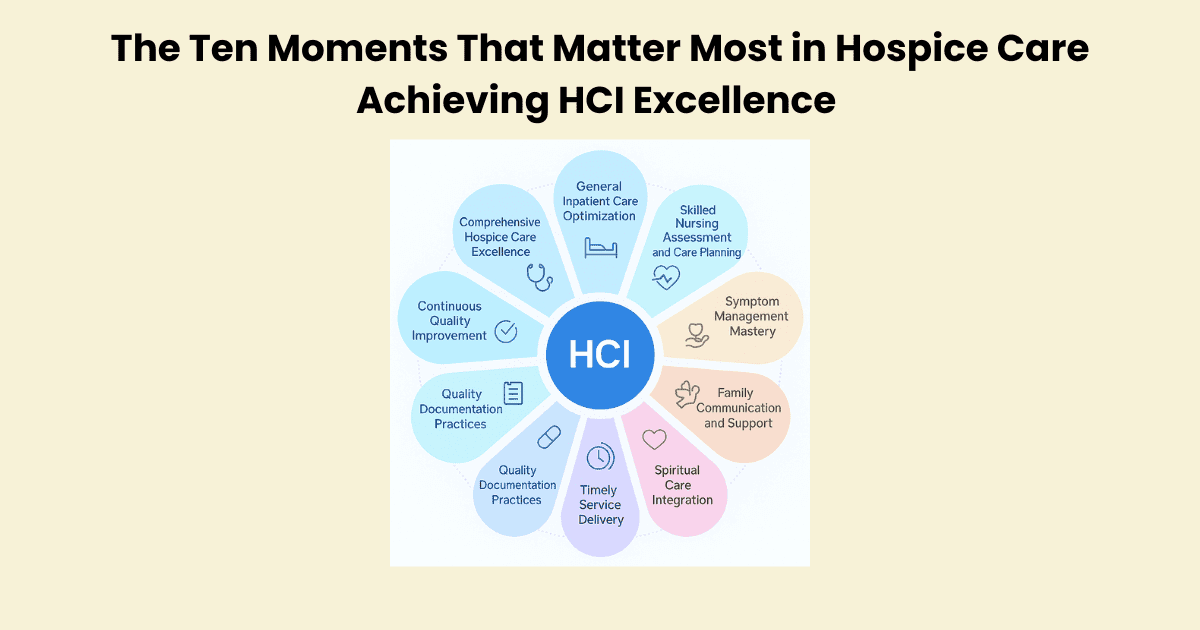
Table of Contents
Picture this: You’re sitting in a meeting room with your hospice team, looking at your latest HCI scores. The numbers stare back at you—7.2, 6.8, 7.5. Good scores, but not great. You know your team provides excellent care, but something is missing. You’re not alone in this struggle.
Across the country, hospice agencies face the same challenge. Perfect HCI scores of 10 feel impossible to reach. Many leaders believe that achieving excellence requires luck, perfect patients, or resources they simply don’t have. But what if there was a different way to think about this challenge?
Jose Escobar, a respected voice in hospice leadership, has spent years studying what separates good hospice agencies from truly exceptional ones. His work reveals a powerful truth: HCI excellence isn’t about luck—it’s about execution.
Escobar developed what he calls the Polaris 10/10 HCI Execution Framework. This isn’t just another quality improvement program. It’s a systematic approach that identifies the ten most critical moments in hospice care—the moments that make or break your HCI scores.
Think of it like this: If you’re a chef trying to create the perfect meal, you don’t randomly throw ingredients together and hope for the best. You follow a proven recipe, pay attention to timing, and focus on the techniques that matter most. Escobar’s framework gives you that recipe for hospice excellence.
His approach recognizes something important about our work: Hospice care is about comfort, not cures. We’re not trying to fix the unfixable. Instead, we’re focused on removing preventable distress while allowing the natural dying process to unfold with dignity and peace.
Whether you’re a hospice executive looking to improve your agency’s performance or a clinician wanting to provide better care, this article serves as your roadmap. We’ll walk through each of the ten moments that matter most, showing you exactly how to execute them with precision and compassion.
For executives, you’ll discover how to create systems that support consistent excellence. You’ll learn to allocate resources effectively and build a culture where high HCI scores become the natural result of excellent care.
For clinicians, you’ll gain practical tools to enhance your daily practice. You’ll understand how your individual actions contribute to overall agency performance while staying true to hospice’s core mission of comfort care.
| What You’ll Learn | How It Helps |
|---|---|
| The ten critical moments in hospice care | Focus your energy on what matters most |
| Systematic execution strategies | Replace guesswork with proven methods |
| Comfort care principles | Align quality metrics with hospice values |
| Practical implementation steps | Turn knowledge into action |
This isn’t about working harder—it’s about working smarter. Every hospice professional wants to provide excellent care. The question is: How do you consistently deliver that excellence in ways that show up in your HCI scores?
The answer lies in understanding that quality hospice care and high HCI scores aren’t separate goals—they’re the same goal. When you focus on the moments that matter most and use a proven framework, excellence becomes achievable.
Your patients and families deserve nothing less than your best. This article will show you how to give it to them, one moment at a time.
The Hospice Care Index (HCI) is a quality measurement tool that helps us understand how well hospice agencies care for patients and families during one of life’s most sacred transitions. Think of it as a report card that measures the things that matter most in hospice care.
The HCI focuses on comfort care principles—the heart of hospice. It doesn’t measure how many patients we “save” because that’s not our mission. Instead, it measures how effectively we remove preventable suffering while supporting the natural dying process with dignity and compassion.
At its core, the HCI asks simple but profound questions: Are we managing pain well? Are families getting the support they need? Are we honoring each person’s wishes for their final days? These aren’t just numbers—they reflect our commitment to excellent end-of-life care.
The HCI uses a straightforward 0-10 scoring system that makes it easy to understand where your agency stands. Here’s how it works:
| Score Range | Performance Level | What This Means |
|---|---|---|
| 9-10 | Exceptional | Outstanding care that consistently exceeds expectations |
| 7-8 | Good | Solid performance with room for improvement |
| 5-6 | Average | Meeting basic standards but missing opportunities |
| 3-4 | Below Average | Significant gaps in care quality |
| 0-2 | Poor | Major concerns requiring immediate attention |
A score of 10 represents perfect execution—every patient received excellent pain management, every family felt supported, and every care plan reflected the patient’s values and wishes. While this might seem impossible to achieve, agencies using systematic approaches like Jose Escobar’s framework are proving it can be done.
The beauty of this system is its simplicity. You don’t need complex calculations or statistical analysis. A higher score means better care; everyone on your team can understand what that means for the families you serve.
The HCI has become a central piece of how hospice quality is measured and reported across the industry. This isn’t just internal data that stays within your agency—it’s information that gets shared with regulatory bodies, payers, and sometimes even the public.
When Medicare evaluates hospice agencies, HCI scores play a significant role in determining quality ratings. These ratings affect everything from reimbursement rates to your agency’s reputation in the community. More importantly, they reflect whether families receive the compassionate, skilled care they deserve during their most vulnerable moments.
Quality reporting through the HCI helps the entire hospice industry improve. When agencies share data about what works and what doesn’t, everyone benefits. Families get better care, and hospice professionals have clearer guidance about best practices.
Every hospice professional knows this truth: When HCI scores are high, patients and families experience better outcomes. This isn’t just about meeting metrics—it’s about real people having more peaceful deaths and families finding comfort during their grief.
High HCI scores typically indicate:
Patient satisfaction surveys consistently show that families served by high-HCI agencies report feeling more supported, better prepared for the dying process, and more confident that their loved one’s final days reflected their values and preferences.
This connection isn’t coincidental. The HCI measures the very things that create positive experiences for patients and families. When you focus on improving your HCI scores, you’re directly improving the quality of care you provide.
Let’s be honest about something: Regulatory compliance in hospice care can feel overwhelming. The HCI helps simplify this challenge by providing a clear framework for meeting many of your most important compliance requirements.
CMS (Centers for Medicare & Medicaid Services) uses HCI data as part of its quality assessment process. Agencies with consistently high HCI scores typically have fewer compliance issues during surveys because they systematically address the core elements of quality hospice care.
| Compliance Area | How HCI Helps |
|---|---|
| Patient Rights | Measures respect for patient autonomy and decision-making |
| Care Planning | Evaluates individualized, comprehensive care approaches |
| Symptom Management | Tracks the effectiveness of pain and symptom control |
| Family Support | Assesses caregiver education and bereavement services |
| Quality Improvement | Provides data for systematic performance enhancement |
Think of HCI compliance as a pathway rather than a burden. When your systems are designed to achieve high HCI scores, you’re naturally addressing most regulatory requirements while staying focused on what matters most—excellent patient care.
In today’s healthcare environment, families have choices about their hospice care. They’re asking harder questions, doing more research, and expecting transparency about quality outcomes. Your HCI scores can be a powerful differentiator in this competitive landscape.
High HCI scores tell a compelling story about your agency’s commitment to excellence. They demonstrate that you’re not just meeting minimum standards—you’re consistently delivering exceptional care that makes a real difference in people’s lives.
Referral sources—physicians, hospitals, and other healthcare providers—are increasingly aware of HCI scores when making recommendations. They want to partner with agencies that consistently deliver excellent outcomes because it reflects their own commitment to quality patient care.
Here’s what competitive advantage through HCI excellence looks like in practice:
Most importantly, focusing on HCI excellence creates a positive cycle. Better scores lead to more referrals, which provide more resources to invest in quality improvement, which leads to even better scores. It’s a sustainable path to both mission fulfillment and business success.
Remember, at the end of the day, HCI scores simply reflect how well we’re honoring our commitment to providing compassionate, skilled care during life’s most sacred transition. When we focus on what these numbers represent—comfort, dignity, and peace for dying patients and their families—improving them becomes a business goal and a moral imperative.
Jose Escobar’s Polaris 10/10 HCI Execution Framework represents a fundamental shift in how hospice agencies approach quality improvement. Rather than treating HCI excellence as a lucky accident or an impossible dream, Escobar’s methodology treats it as an achievable outcome through deliberate, systematic action.
The framework gets its name from the North Star—Polaris—which has guided travelers for centuries. Just as sailors use this constant star to navigate treacherous waters, hospice agencies can use this framework to navigate the complex journey toward perfect HCI scores. The “10/10” represents both the perfect HCI score and the ten critical moments that make that score possible.
Escobar developed this approach after studying hundreds of hospice agencies and identifying the patterns that separate high-performing organizations from those struggling with mediocre results. He discovered that excellent agencies weren’t just lucky—they were doing specific things at specific times in very specific ways.
This methodology is unique because it focuses on precision execution during the moments that matter most. Instead of trying to improve everything at once, the framework identifies the ten pivotal moments in hospice care where excellence significantly impacts HCI scores and patient outcomes.
The Polaris 10/10 Framework is built on five core principles that align perfectly with hospice’s mission of comfort care:
Principle 1: Comfort First, Metrics Second
The framework recognizes that good metrics naturally follow when you focus on removing preventable distress and honoring patient wishes. High HCI scores result from excellent comfort care, not the goal itself.
Principle 2: Systematic Execution Over Random Efforts
Excellence doesn’t happen by accident. It requires deliberate, consistent execution of proven practices at the right time and in the right way. Every action should be purposeful and aligned with the overall framework.
Principle 3: Moments Matter More Than Marathons
Instead of always trying to be perfect, the framework focuses on ten critical moments where excellence has the greatest impact. Perfect execution during these moments creates exceptional outcomes.
Principle 4: Build Systems, Don’t Rely on Heroes
High-performing agencies don’t depend on a few exceptional individuals. They create systems and processes that enable every team member to deliver excellent care consistently.
Principle 5: Continuous Improvement Through Structured Learning
The framework includes built-in mechanisms for learning from both successes and failures. Every interaction becomes an opportunity to refine and improve the approach.
| Traditional Approach | Polaris 10/10 Framework |
|---|---|
| Random quality improvement efforts | Systematic focus on ten critical moments |
| Hoping for better outcomes | Building systems that ensure better outcomes |
| Reactive problem-solving | Proactive excellence execution |
| Individual heroics | Team-based systematic approach |
| Metrics-driven decisions | Comfort-driven decisions that improve metrics |
The path from average to exceptional HCI performance isn’t a straight line—it’s a carefully planned journey with distinct phases that build on each other. Understanding this journey helps hospice leaders set realistic expectations and maintain momentum during challenging periods.
Phase 1: Foundation Building (Months 1-3)
This phase focuses on establishing the basic infrastructure needed for systematic excellence. Teams learn the ten critical moments, understand their roles, and begin practicing new approaches in low-risk situations. Don’t expect dramatic HCI improvements yet—this phase is about building the foundation for future success.
Phase 2: Skill Development (Months 4-9)
During this phase, teams develop competency and confidence in executing the framework. Though overall HCI scores may still fluctuate, you’ll start seeing improvements in individual moments. This is normal and expected—skill development takes time and practice.
Phase 3: Integration and Consistency (Months 10-15)
The framework becomes second nature to your team. All ten moments are being executed consistently, and you’ll see steady improvements in HCI scores. This phase requires patience and persistence—the results are building, even when they’re not always visible.
Phase 4: Optimization and Excellence (Months 16+)
Your team has mastered the framework and is fine-tuning execution based on their unique patient population and organizational culture. HCI scores of 9-10 become the norm rather than the exception.
The key insight from Escobar’s work is that exceptional performance is a process, not an event. Agencies that try to skip phases or rush the journey often fail because they haven’t built the necessary foundation for sustained excellence.
The difference between agencies that achieve HCI excellence and those that don’t often comes down to mindset and approach. Struggling agencies typically “wish” for better outcomes, while exceptional agencies “build” systems that create those outcomes.
The Building Mindset treats HCI improvement as a construction project. For the project to succeed, you need blueprints (the framework), the right materials (training and resources), skilled workers (your team), and quality control processes (monitoring and feedback). Every element must be in place and working together.
Here’s what systematic HCI improvement looks like in practice:
Clear Standards and Expectations
Every team member understands exactly what excellent execution looks like for each of the ten critical moments. These aren’t vague guidelines—they’re specific, measurable standards that guide daily practice.
Consistent Training and Development
Teams receive ongoing education and skill development focused on the framework’s requirements. This isn’t a one-time training event—it’s a continuous learning process that evolves with your agency’s growth.
Regular Monitoring and Feedback
Performance is tracked and discussed regularly, with specific feedback about what’s working well and what needs improvement. This creates a culture of continuous improvement rather than reactive problem-solving.
Structured Problem-Solving
When issues arise, they’re addressed systematically using the framework’s principles rather than through random interventions. This ensures that solutions align with the overall approach and contribute to long-term success.
Many hospice agencies make the mistake of approaching HCI improvement through random quality improvement efforts. They might focus on documentation one month, pain management the next, and family communication after that. While these are all critical areas, this scattered approach rarely produces lasting improvements.
Random efforts fail because they:
Lack of Strategic Focus
Without a clear framework, agencies chase multiple priorities simultaneously. Teams become overwhelmed and confused about what matters most, leading to inconsistent execution across all areas.
Miss Critical Connections
The ten moments in hospice care are interconnected. Poor execution in one moment affects all the others. Random efforts fail to account for these connections, creating gaps that undermine overall performance.
Create Temporary Improvements
Random efforts might produce short-term gains, but don’t build the systematic capabilities needed for sustained excellence. When attention shifts to the next priority, previous improvements often disappear.
Exhaust Team Resources
Constantly changing priorities and approaches drain team energy and motivation. Staff become cynical about quality improvement efforts because they’ve seen too many initiatives fail.
Generate Inconsistent Results
Without systematic execution, outcomes become unpredictable. Good results feel accidental, and poor results feel inevitable. This creates a sense of helplessness that undermines team confidence.
Structured execution is the bridge between good intentions and excellent outcomes. It’s the difference between knowing what to do and actually doing it consistently, especially during stressful situations when natural instincts might lead to shortcuts.
What Structured Execution Looks Like:
Defined Processes for Each Moment
Clear, step-by-step processes guide team members through optimal execution at every critical moment. These processes are detailed enough to ensure consistency but flexible enough to accommodate individual patient needs.
Built-in Quality Checkpoints
The framework includes regular checkpoints where teams assess their execution and adjust as needed. These aren’t punitive evaluations—they’re learning opportunities that help teams improve.
Escalation Procedures
When challenges arise, teams have clear procedures for getting help and additional resources. This ensures that problems are addressed quickly before they affect patient care or HCI scores.
Continuous Refinement
The framework includes mechanisms for ongoing improvement based on real-world experience. Teams regularly review what’s working well and what could be enhanced, ensuring that the approach evolves with changing needs.
| Random Efforts | Structured Execution |
|---|---|
| Scattered focus on multiple priorities | Strategic focus on ten critical moments |
| Inconsistent application of improvements | Systematic execution of proven practices |
| Temporary gains that fade over time | Sustained improvements that build on each other |
| Team exhaustion from constant change | Team confidence from consistent success |
| Unpredictable outcomes | Reliable, excellent results |
The truth is simple: Wishing for better HCI scores won’t make them happen. Building the systems, skills, and processes that create excellent outcomes will. The Polaris 10/10 Framework provides the blueprint for that construction project, but success depends on your commitment to systematic execution rather than hopeful thinking.
Remember, every family deserves excellent hospice care, and every hospice professional wants to provide it. The framework provides the tools to make that excellence predictable and sustainable rather than accidental and temporary.
These ten moments represent the critical touchpoints where excellent execution directly impacts your HCI scores and, more importantly, the quality of care your patients receive. Each moment offers an opportunity to demonstrate hospice’s core mission: allowing the body to die naturally while removing as much preventable distress as possible.
Comprehensive Hospice Care is the foundation of everything else that follows. When patients need continuous care that can’t be provided in their home, CHC bridges the gap between routine home care and inpatient services. The key to CHC excellence is clear clinical justification demonstrating medical necessity.
Your clinical justification must answer three essential questions: Why does this patient need continuous care? Why can’t this care be provided through routine visits? What specific interventions will be provided during the CHC period?
Strong clinical justification includes:
Documentation for CHC must tell a complete story that any reviewer can understand. Your notes should paint a clear picture of why continuous care was necessary and how it improved the patient’s comfort and dignity.
| Documentation Element | What to Include |
|---|---|
| Clinical Status | Specific symptoms, vital signs, and level of consciousness |
| Interventions Provided | Medications given, comfort measures, and family support |
| Response to Care | How the patient responded to interventions |
| Ongoing Assessment | Changes in condition, new symptoms, evolving needs |
| Caregiver Support | Education provided, emotional support given |
Remember: Your documentation serves multiple purposes. It justifies the level of care, guides other team members, and demonstrates your commitment to excellent patient care.
Excellent CHC delivery requires both clinical skills and emotional intelligence. You’re not just managing symptoms—you’re providing peace of mind to families during their most vulnerable moments.
Clinical excellence in CHC means:
Emotional excellence in CHC means:
GIP care represents the highest level of hospice service, reserved for situations where symptoms can’t be managed in other settings. The decision to recommend GIP care requires careful assessment and clear criteria prioritizing patient comfort while ensuring appropriate resource utilization.
GIP is appropriate when:
GIP is not appropriate for:
Successful GIP care requires seamless coordination between your hospice team and the facility providing the care. This coordination ensures that the patient’s comfort remains the priority while maintaining continuity with their established care plan.
Effective coordination includes:
Key coordination checkpoints:
Quality GIP care is measured by specific indicators reflecting clinical excellence and patient satisfaction. These indicators help you assess whether your GIP services meet their intended goals.
| Quality Indicator | What to Measure | Excellence Standard |
|---|---|---|
| Symptom Control | Pain and symptom scores | 90% of patients report comfort within 24 hours |
| Length of Stay | Average GIP duration | Appropriate to clinical need, not extended unnecessarily |
| Transition Success | Smooth return to home care | 95% of patients successfully transitioned back |
| Family Satisfaction | Family feedback scores | High satisfaction with communication and care |
Your initial assessment sets the foundation for everything that follows in the patient’s hospice journey. This isn’t just a checklist to complete—it’s your opportunity to understand the whole person and create a care plan that honors their values, preferences, and goals.
Comprehensive initial assessment includes:
The assessment should answer these critical questions:
Care plans are living documents that evolve with the patient’s changing needs. Excellent care plan management means regular reassessment and adjustment that keeps the plan relevant and effective.
Effective care plan management includes:
Care plan reviews should happen:
Hospice care works best when the entire team works together seamlessly. As the primary clinical coordinator, you are crucial in ensuring that all team members understand the patient’s needs and contribute their expertise effectively.
Successful team coordination requires:
| Team Member | Primary Role | Coordination Needs |
|---|---|---|
| Physician | Medical management | Treatment plans, medication changes |
| Social Worker | Psychosocial support | Family dynamics, resource needs |
| Chaplain | Spiritual care | Spiritual concerns, ritual needs |
| Aide | Personal care | Care preferences, safety concerns |
| Volunteer | Companionship | Emotional support, practical help |
Pain management is often the first concern families have when choosing hospice care. Excellent pain control requires clinical expertise and compassionate understanding of what pain means to each patient.
Effective pain assessment includes:
Pain management strategies should be:
Key principles for pain management:
Shortness of breath can be one of the most frightening symptoms for patients and families. Effective dyspnea management requires both clinical interventions and emotional support that helps patients and families feel more in control.
Dyspnea assessment should include:
Management strategies include:
Systematic symptom tracking helps you identify patterns and adjust care plans for maximum effectiveness. This isn’t just about documenting symptoms—it’s about continuously using that information to improve patient comfort.
Effective symptom tracking includes:
| Symptom | Assessment Frequency | Key Tracking Points |
|---|---|---|
| Pain | Every visit | Location, intensity, duration, and relief measures |
| Dyspnea | Every visit | Severity, triggers, positioning, and oxygen needs |
| Nausea | Daily if present | Timing, triggers, appetite impact, and medication response |
| Anxiety | Weekly or as needed | Triggers, severity, coping strategies, support needs |
| Constipation | Every visit | Frequency, comfort, interventions, prevention |
Talking about death and dying requires special skills that combine honesty with compassion. These conversations can be some of the most meaningful interactions you have with families, providing them with the information and emotional support they need during this difficult time.
Effective end-of-life conversations include:
Key communication principles:
Family caregivers are often the unsung heroes of hospice care, providing round-the-clock support while managing their own grief and stress. Regular caregiver burden assessment helps you identify when additional support is needed.
Signs of caregiver burden include:
Support strategies for overburdened caregivers:
Preparing families for bereavement begins long before death occurs. This preparation helps families develop coping strategies and identify support resources needed during their grief journey.
Bereavement preparation includes:
Key topics to address:
Spiritual care is an essential component of hospice care that addresses the deeper questions and concerns that arise when facing death. This care isn’t limited to religious services—it encompasses all aspects of meaning, purpose, and connection that give life significance.
Holistic spiritual care includes:
Spiritual care benefits:
Systematic spiritual assessment helps you understand each patient’s unique spiritual needs and preferences. This assessment guides your referrals to chaplains and your own spiritual care interventions.
Key spiritual assessment areas:
Questions that guide spiritual assessment:
Chaplains bring specialized expertise in spiritual care that complements your nursing skills. Effective coordination with chaplain services ensures that patients receive comprehensive spiritual support that addresses their deepest needs.
Appropriate chaplain referrals include:
Coordination with chaplain services includes:
Medication management in hospice requires a different approach than traditional medical care. The goal isn’t to treat diseases or extend life—it’s to maximize comfort and quality of life while minimizing side effects and medication burden.
Hospice prescribing principles:
Key considerations for hospice prescribing:
Medication reconciliation ensures patient safety by identifying and resolving discrepancies between what patients are supposed to be taking and what they’re actually taking. This process is especially important in hospice care, where medication changes are common.
Effective medication reconciliation includes:
Medication reconciliation should occur:
Hospice agencies must balance excellent care with financial sustainability. Effective formulary management ensures that patients receive the medications they need while controlling costs through strategic decision-making.
Cost-effective formulary principles:
| Medication Category | Cost-Effective Strategies | Quality Considerations |
|---|---|---|
| Pain Management | Generic opioids, bulk purchasing | Ensure adequate pain relief |
| Anxiety/Agitation | Generic benzodiazepines, alternatives | Monitor for effectiveness |
| Nausea/Vomiting | Generic antiemetics, combination therapy | Prevent breakthrough symptoms |
| Constipation | Generic laxatives, prevention protocols | Maintain bowel function |
| Respiratory | Generic bronchodilators, oxygen therapy | Optimize breathing comfort |
The right visit frequency balances patient needs with resource utilization while ensuring that patients receive the care they need when they need it. This requires careful assessment and ongoing adjustment based on patient condition and family needs.
Factors that influence visit frequency:
Visit frequency guidelines:
Timely responses to patient and family calls demonstrate your commitment to excellent care and provide reassurance during difficult times. Clear response time standards help staff prioritize calls and ensure appropriate care.
Response time standards should address:
Typical response time standards:
Crisis situations require immediate, skilled intervention that addresses both clinical needs and family anxiety. Clear protocols help staff respond effectively while maintaining focus on comfort care principles.
Common crisis situations:
Crisis intervention protocols should include:
Documentation in hospice care serves multiple purposes: it demonstrates the quality of care provided, ensures regulatory compliance, and communicates essential information to other team members. Excellent documentation tells the story of your patient’s journey and your professional response to their needs.
Compliance-based documentation must demonstrate:
Key documentation principles:
The HOPE tool represents a significant advancement in hospice quality measurement. It provides a standardized assessment and documents patient-centered outcomes. Successful HOPE integration requires understanding both the technical requirements and the clinical value of this assessment tool.
The comprehensive resources “HOPE in Practice: Implementing Patient-Centered Outcomes in Hospice Care“ and “HOPE in Action: A Practical Guide to Hospice Assessments“ provide detailed guidance for implementing HOPE assessments effectively in your clinical practice.
HOPE assessment components include:
Best practices for HOPE integration:
Audit-ready documentation means your records can withstand scrutiny while telling a compelling story about the excellent care you provide. This requires attention to detail, consistency, and a thorough understanding of what auditors look for.
Audit-ready records demonstrate:
Documentation best practices:
| Documentation Element | What Auditors Look For | Best Practice Tips |
|---|---|---|
| Assessment | Comprehensive, skilled evaluation | Use specific measurements and observations |
| Interventions | Skilled nursing actions | Explain why you chose specific interventions |
| Response | Patient outcomes and changes | Document both improvement and continued needs |
| Education | Family teaching and understanding | Include what was taught and how family responded |
| Coordination | Team communication and planning | Show how you worked with other disciplines |
Continuous quality improvement requires systematic use of data to identify opportunities, implement changes, and measure results. This isn’t about blame or punishment—it’s about using information to provide better care for patients and families.
Effective improvement cycles include:
Key data sources for improvement:
Ongoing education ensures your team has the skills and knowledge to provide excellent care. This education should be practical, relevant, and directly connected to improving patient outcomes and HCI scores.
Effective staff education includes:
Training priorities should focus on:
Measuring outcomes helps you understand whether your improvement efforts are making a difference in patient care. This measurement should be systematic, regular, and focused on what matters most to patients and families.
Key outcomes to measure:
Effective outcome measurement includes:
Response to outcome data should be:
Remember, these ten moments are interconnected. Excellence in one area supports excellence in all areas, creating a comprehensive approach to hospice care that truly honors the dignity and comfort of every patient and family you serve. The goal isn’t just higher HCI scores—it’s better care reflecting what hospice can offer during life’s most sacred transition.
Success in achieving HCI excellence requires different approaches for different roles within your organization. Each level of leadership has unique responsibilities and opportunities to drive improvement. The key is ensuring that every person understands their role in creating the systematic excellence that leads to better patient care and higher HCI scores.
Your role as an executive is to create the vision and provide the resources necessary for HCI excellence. This means thinking beyond quarterly results to build sustainable systems that support long-term success.
Effective strategic planning for HCI improvement begins with understanding your current position. You need to know where your agency stands today before you can plan where it needs to go tomorrow. This requires honest assessment of your strengths, weaknesses, and opportunities for improvement.
Key strategic planning elements include:
Remember that strategic planning for HCI improvement is different from other business initiatives. This isn’t about increasing market share or reducing costs—it’s about creating systems that consistently deliver excellent comfort care while naturally producing high HCI scores.
Money follows priorities, and your budget decisions communicate your true priorities to your entire organization. Successful HCI improvement requires thoughtful investment in the right areas at the right time.
Priority areas for resource allocation:
Staff Development and Training
Your team is your most valuable resource for HCI improvement. Investing in their skills and knowledge directly impacts patient care quality. This includes both clinical training and soft skills development, such as communication and emotional intelligence.
Technology and Systems
Modern hospice care requires technology that supports rather than hinders excellent care. Invest in systems that allow staff to focus on patients rather than administrative tasks.
Quality Improvement Infrastructure
You need dedicated resources for measuring, analyzing, and improving HCI performance. This might include quality improvement staff, data analysis tools, and regular performance review processes.
| Investment Area | Expected ROI | Timeline for Results |
|---|---|---|
| Staff Training | Higher HCI scores, better patient satisfaction | 6-12 months |
| Technology Upgrades | Improved efficiency, better documentation | 3-6 months |
| Quality Infrastructure | Systematic improvement, sustained excellence | 12-18 months |
| Leadership Development | Better team performance, reduced turnover | 6-12 months |
Your staff’s success determines your agency’s success. Staff development isn’t just about meeting regulatory requirements—it’s about creating a team that consistently delivers excellent care under pressure.
Effective staff development includes:
The most successful hospice agencies view staff development as an investment rather than an expense. They understand that skilled, confident staff provide better care and improve patient and family outcomes.
Technology should support your mission, not complicate it. The right technology makes it easier for staff to provide excellent care, while the wrong technology creates barriers and frustration.
Key technology considerations for HCI improvement:
Technology integration should be planned carefully with input from the staff who will use it daily. The best technology in the world won’t help if your team doesn’t use it effectively.
You can’t improve what you don’t measure. Effective performance monitoring gives you the information you need to make informed decisions about your HCI improvement efforts.
Key performance indicators should include:
Dashboard development makes it easier to track multiple indicators simultaneously and identify patterns that might not be obvious when looking at individual metrics.
Regular review processes ensure that performance data gets translated into action. Data without action is just interesting information—it doesn’t improve patient care.
As a clinical manager, you bridge executive vision and frontline reality. Your role is to translate strategic goals into practical actions that staff can implement in their daily work.
Operational excellence means creating systems and processes that make it easy for staff to do the right thing consistently. This requires understanding both the clinical requirements and the practical realities of hospice care delivery.
Efficient workflows allow staff to spend more time with patients and less time on administrative tasks. This directly impacts both job satisfaction and the quality of care provided.
Key workflow optimization strategies:
Workflow optimization should involve the staff who do the work daily. They often have the best ideas for improvement because they understand the practical challenges and opportunities.
Effective training programs do more than meet regulatory requirements—they build the skills and confidence that enable excellent patient care.
Training programs should be:
The most effective training combines formal education with practical application. Staff learn best when they can immediately apply new knowledge and skills to their work.
Quality assurance isn’t about catching mistakes—it’s about preventing them. Effective protocols help staff maintain high standards consistently while providing support when challenges arise.
Quality assurance should include:
| Quality Measure | Review Frequency | Responsible Party |
|---|---|---|
| Pain Management | Every visit | Direct care staff |
| Care Plan Updates | Weekly | Clinical managers |
| Family Satisfaction | Monthly | Quality team |
| Documentation Quality | Quarterly | Clinical managers |
| HCI Performance | Quarterly | Executive team |
Strong teams provide better care than collections of individuals. Team development focuses on building the relationships, communication, and collaboration that enable excellent patient care.
Competency building ensures that every team member has the skills needed to contribute effectively to HCI excellence. This goes beyond basic clinical skills, including communication, problem-solving, and teamwork abilities.
Competency building should address:
Competency building is an ongoing process that adapts to changing needs and new challenges. Regular assessment helps identify areas for additional development.
Clear communication is essential for coordinated care and positive patient outcomes. This includes communication within the team, with patients and families, and with external partners.
Communication enhancement strategies:
Hospice care works best when all disciplines work together seamlessly. This requires understanding each team member’s role and how they contribute to overall patient care.
Effective interdisciplinary collaboration includes:
As a direct care provider, you have the most immediate impact on patient comfort and HCI scores. Your clinical skills, compassion, and attention to detail directly affect every family you serve.
Clinical excellence in hospice care means consistently providing comfort-focused care that honors each patient’s values and preferences while managing symptoms effectively.
Skilled assessment is the foundation of excellent hospice care. Your ability to accurately assess patient needs, symptoms, and responses to treatment directly impacts care quality and patient outcomes.
Key assessment skills include:
Assessment skills improve with practice and feedback. Regular case discussions and peer review help you refine your assessment abilities and learn from challenging situations.
Your documentation tells the story of your patient’s journey and demonstrates the excellent care you provide. Quality documentation supports both patient care and regulatory compliance.
Documentation improvement strategies:
Remember that documentation serves multiple purposes—it guides other team members, justifies the care provided, and demonstrates your professional competence.
Patient advocacy means ensuring that each patient’s voice is heard and their preferences are honored throughout their hospice journey. This requires both clinical skills and emotional intelligence.
Effective patient advocacy includes:
Continuing your professional growth benefits both you and the patients you serve. Professional development keeps your skills current and prepares you for increased responsibilities.
Continuing education should be strategic and focused on areas that benefit your practice and your patients most.
Priority areas for continuing education:
Professional certifications demonstrate your commitment to excellence and provide structure for ongoing learning. Maintaining certifications requires planning and dedication.
Certification maintenance strategies:
Learning from colleagues is one of the most effective ways to improve your practice and develop new skills. Peer learning creates a culture of continuous improvement.
Peer learning opportunities include:
| Development Activity | Time Investment | Expected Benefit |
|---|---|---|
| Formal education courses | 20-40 hours | New knowledge and skills |
| Peer learning sessions | 2-4 hours monthly | Practical tips and support |
| Professional conferences | 16-24 hours annually | Networking and latest practices |
| Mentoring relationships | 1-2 hours weekly | Personalized growth guidance |
| Quality improvement projects | Variable | System improvement skills |
Remember that professional development isn’t just about meeting requirements—it’s about becoming the kind of healthcare provider who can make a real difference in people’s lives during their most vulnerable moments. Your commitment to excellence honors the trust that patients and families place in you during their journey with hospice care.
The path to HCI excellence requires commitment from everyone in your organization. When executives provide vision and resources, clinical managers create supportive systems, and direct care staff deliver excellent care, the result is an organization that consistently achieves both high HCI scores and exceptional patient outcomes. This isn’t just about metrics—it’s about fulfilling hospice’s sacred mission of providing comfort, dignity, and peace during life’s final chapter.
Improving HCI scores isn’t just about reaching a number—it’s about creating better experiences for patients and families during one of life’s most sacred transitions. When you measure success thoughtfully, you’re not just tracking metrics but honoring your commitment to excellent comfort care.
Before you can improve, you need to know where you stand today. This honest assessment isn’t about blame or judgment—it’s about understanding your current reality so you can create a meaningful path forward.
Your baseline assessment should capture the full picture of your agency’s performance. This means looking at HCI scores, but also understanding the deeper factors that create those scores.
Key areas to evaluate:
Remember that the baseline assessment is a snapshot in time. Your goal isn’t to judge past performance but to create a foundation for future improvement. Approach this process with curiosity rather than criticism.
The most valuable baseline assessments include both quantitative data and qualitative insights. Numbers tell you what’s happening, but stories from patients, families, and staff tell you why it’s happening.
Gap analysis helps you identify the specific areas where your current performance differs from your desired outcomes. This systematic approach prevents you from trying to fix everything at once.
Effective gap analysis asks these critical questions:
Gap analysis should be systematic and objective. Use data whenever possible, but don’t ignore the insights that come from experience and observation.
| Performance Area | Current Score | Target Score | Gap Size | Priority Level |
|---|---|---|---|---|
| Pain Management | 7.2 | 9.5 | 2.3 | High |
| Family Communication | 8.1 | 9.0 | 0.9 | Medium |
| Symptom Control | 6.8 | 9.0 | 2.2 | High |
| Spiritual Care | 7.9 | 8.5 | 0.6 | Low |
| Caregiver Support | 7.5 | 9.0 | 1.5 | Medium |
The most important gaps aren’t always the largest ones. Sometimes, a small gap in a critical area has more impact on patient comfort than a large gap in a less essential area.
Not all gaps are created equal. Effective priority setting ensures that your improvement efforts focus on the areas that will most impact patient comfort and HCI scores.
Priority setting should consider:
Use a systematic approach to priority setting that combines data with professional judgment. The goal is to focus your energy on the changes that will make the biggest difference for patients and families.
High-priority improvements typically:
Remember that priority setting is an ongoing process. As you improve in some areas, new priorities may emerge. Stay flexible and responsive to changing needs.
Consistent monitoring helps you understand whether your improvement efforts are working. This isn’t about creating more paperwork—it’s about ensuring that changes in practice translate into better patient outcomes.
Effective score tracking includes:
The frequency of tracking should match the pace of change. Some improvements happen quickly, while others take time to develop. Adjust your monitoring schedule to capture meaningful progress without overwhelming your team.
Make tracking data accessible and understandable to everyone involved in improvement efforts. When staff can see how their efforts affect patient outcomes, they’re more motivated to maintain high standards.
Individual scores tell you what happened, but trends tell you what’s happening. Trend analysis helps you understand whether improvements are sustainable and identify areas that need additional attention.
Effective trend analysis looks for:
Visual representation of trends makes it easier to spot patterns and communicate progress to your team. Simple charts and graphs can reveal insights that aren’t obvious in raw data.
Don’t overreact to short-term fluctuations. HCI improvement is a long-term process that requires patience and persistence. Focus on sustained trends rather than month-to-month variations.
When monitoring reveals problems or setbacks, swift corrective action prevents small issues from becoming major challenges. This proactive approach maintains momentum and demonstrates your commitment to excellence.
Effective corrective action planning includes:
Corrective action should be proportional to the problem. Small issues may require minor adjustments, while significant problems may need comprehensive intervention.
The best corrective actions strengthen your overall improvement system rather than just fixing immediate problems. Look for solutions that prevent similar issues in the future.
| Problem Type | Response Time | Action Level | Follow-up Schedule |
|---|---|---|---|
| Individual patient concern | Immediate | Direct intervention | 24-48 hours |
| Staff performance issue | 1-2 days | Coaching/training | Weekly for 1 month |
| System/process problem | 1 week | Process improvement | Monthly for 3 months |
| Trend deterioration | 2 weeks | Comprehensive review | Quarterly assessment |
Celebrating progress is just as important as identifying problems. Recognition reinforces positive behaviors and motivates continued excellence. This isn’t about participation trophies—it’s about acknowledging meaningful improvements that benefit patients and families.
Meaningful milestones to celebrate include:
Recognition should be timely, specific, and connected to your comfort care mission. Help your team understand how their efforts translate into better patient experiences.
Different achievements call for different types of recognition. A small improvement might warrant an acknowledgment in a team meeting, while a major breakthrough might deserve a special celebration.
The most powerful recognition connects individual efforts to patient outcomes. When staff see how their work affects real families, the recognition becomes more meaningful and motivating.
Sustained HCI improvement requires sustained motivation. Your team needs to see that their efforts matter and that progress is possible even when change feels slow.
Effective motivation strategies include:
Motivation must be authentic and consistent. Empty praise or inconsistent recognition can actually damage morale. Focus on genuine appreciation for meaningful contributions.
The strongest motivation comes from seeing the impact of your work on patients and families. Share stories, letters, and feedback that demonstrate how excellent care makes a difference.
Remember that different people are motivated by different things. Some staff respond to public recognition, while others prefer private acknowledgment. Tailor your approach to individual preferences and cultural considerations.
Real success means creating improvements that last. Sustainability planning ensures that your HCI gains continue even when attention shifts to other priorities.
Sustainable improvement requires:
Sustainability planning should begin during the improvement process, not after goals are achieved. Build sustainability into your improvement efforts from the beginning.
The most sustainable improvements become part of your agency’s DNA. They’re not special programs or initiatives—they’re simply how you do business.
| Sustainability Element | Implementation Strategy | Success Indicator |
|---|---|---|
| Staff Competency | Ongoing training and development | Consistent performance across all staff |
| Process Integration | Standard procedures and protocols | Automatic execution of best practices |
| Leadership Support | Regular review and resource allocation | Continued investment in improvement |
| Cultural Adoption | Values-based decision making | Improvement happens without enforcement |
| Continuous Learning | Regular assessment and adjustment | Proactive identification of new opportunities |
Remember that sustainability doesn’t mean standing still. The most sustainable improvements create a foundation for continuous growth and enhancement.
Your ultimate measure of success isn’t just higher HCI scores—it’s the knowledge that more patients are experiencing comfort, dignity, and peace during their final journey. When you measure success thoughtfully, celebrate achievements meaningfully, and plan for sustainability systematically, you’re not just improving metrics. You’re fulfilling hospice’s sacred promise to provide excellent comfort care when families need it most.
The path to HCI excellence is challenging, but it’s also deeply rewarding. Every improvement you make, every milestone you achieve, and every system you strengthen contributes to a legacy of compassionate care that honors both the patients you serve and the professionals who dedicate their lives to this meaningful work.
Every hospice agency faces obstacles on its journey to HCI excellence. The good news is that these challenges are predictable and manageable when approached with the right strategies and mindset. Remember, overcoming these challenges isn’t just about improving scores—it’s about creating better systems that serve patients and families during their most vulnerable moments.
Limited resources don’t have to mean limited excellence. The most successful hospice agencies have learned to maximize impact with available resources by focusing on high-value activities and eliminating waste.
Resource constraints often force innovation, leading to better, more efficient care delivery. When you can’t throw money at problems, you find creative solutions that frequently work better than expensive alternatives.
Key principles for creative solution development:
Examples of creative solutions:
The most creative solutions often come from frontline staff who understand the daily challenges and opportunities. Create systems that encourage and reward innovative thinking from all levels of your organization.
You don’t have to fix everything at once. Phased implementation allows you to make meaningful progress with limited resources while building momentum for future improvements.
Effective phased implementation starts with the changes that will immediately impact patient comfort and HCI scores. This creates early wins that build confidence and support for additional phases.
Phase 1: Foundation Building (Months 1-6)
Focus on the most critical elements that affect patient comfort:
Phase 2: Skill Development (Months 7-12)
Build on the foundation with more advanced capabilities:
Phase 3: Optimization (Months 13-18)
Fine-tune your systems for consistent excellence:
| Phase | Resource Investment | Expected Outcomes | Key Success Factors |
|---|---|---|---|
| Foundation | Low to moderate | Improved basic care quality | Staff buy-in, leadership support |
| Skill Development | Moderate | Enhanced capabilities | Consistent training, practice opportunities |
| Optimization | Moderate to high | Sustained excellence | System integration, continuous learning |
The key to successful phased implementation is patience and persistence. Don’t skip phases or rush the process—each phase builds essential capabilities needed for the next level of performance.
Every improvement initiative should demonstrate clear value for both patient outcomes and organizational sustainability. Cost-benefit analysis helps you make informed decisions about resource allocation.
Cost-benefit analysis for HCI improvement considers:
Simple cost-benefit framework:
Remember that some benefits are difficult to quantify but extremely valuable. The peace of mind that comes from excellent pain management, the comfort that families feel from good communication, and the professional satisfaction that staff experience from meaningful work all contribute to success even when they’re hard to measure.
Focus on improvements that provide both immediate relief and long-term value. The best investments in HCI improvement pay dividends in patient comfort, staff satisfaction, and organizational sustainability.
Change is hard, even when it’s good. Staff resistance often comes from fear, uncertainty, or past negative experiences with change initiatives. Understanding the root causes of resistance helps you address concerns effectively.
Common reasons for staff resistance:
Effective change management strategies address these concerns directly:
Involve staff in planning and implementation. When people help create solutions, they’re more likely to support them. Ask for input, listen to concerns, and incorporate feedback into your improvement plans.
Communicate the “why” behind changes. Help staff understand how improvements will benefit patients and make their work more meaningful. Connect changes to your mission and values.
Provide adequate training and support. Ensure that staff have the skills and resources they need to succeed. Offer multiple learning opportunities and ongoing support as they adapt to new approaches.
Start with willing participants. Some staff members are naturally more open to change. Use early adopters as champions who can help influence others through their positive experiences.
Celebrate small wins along the way. Recognition and acknowledgment of progress help maintain momentum and demonstrate that changes work.
Clear, consistent communication is essential for overcoming resistance and supporting HCI improvement initiatives. Your communication should be honest, empathetic, and focused on patient benefit.
Effective communication techniques include:
Two-way communication that encourages questions and feedback rather than one-way information delivery. Create safe spaces where staff can express concerns without fear of retaliation.
Multiple communication channels to reach different people in ways that work for them. Some staff prefer written updates, others respond better to face-to-face discussions, and some like group meetings.
Consistent messaging that reinforces key points without being repetitive. Everyone should hear the same information about goals, expectations, and progress.
Storytelling that illustrates how changes benefit real patients and families. Specific examples are more powerful than general statements about improvement.
Regular updates about progress, challenges, and adjustments. Keep communication ongoing rather than limiting it to major announcements.
| Communication Method | Best Used For | Frequency | Key Success Factors |
|---|---|---|---|
| Team meetings | Updates, problem-solving | Weekly | Interactive, focused agenda |
| Written updates | Detailed information | Monthly | Clear, concise, actionable |
| One-on-one discussions | Individual concerns | As needed | Private, supportive, honest |
| Success stories | Motivation, examples | Ongoing | Specific, patient-focused |
| Training sessions | Skill development | Scheduled | Practical, relevant, engaging |
People support what they help create and what benefits them. Effective incentive alignment ensures that individual success contributes to organizational success and improved patient outcomes.
Incentive alignment strategies include:
Professional development opportunities that help staff grow their skills and advance their careers. Invest in your people and they’ll invest in your mission.
Recognition programs that acknowledge excellent performance and contribution to HCI improvement. Public recognition can be more motivating than financial rewards.
Autonomy and empowerment give staff meaningful control over their work. Trust your team to make good decisions within clear guidelines.
Meaningful work connections that help staff see how their efforts benefit patients and families. Regular feedback from patients and families can be incredibly motivating.
Fair workload distribution that ensures improvement efforts don’t create an unreasonable burden on any individual. Spread the work so everyone can contribute without being overwhelmed.
Performance expectations that are clear, achievable, and directly connected to patient comfort and HCI improvement. Set people up for success rather than failure.
The most effective incentives are intrinsic rather than external. When staff feels proud of their work, confident in their abilities, and connected to their mission, they naturally strive for excellence.
Regulatory requirements change frequently and can significantly impact your HCI improvement efforts. Staying current isn’t just about avoiding penalties—it’s about ensuring that your excellence efforts align with regulatory expectations.
Strategies for staying current:
Designate specific staff members to monitor regulatory updates and communicate changes to the team. Don’t rely on informal information sharing—create systematic processes for staying informed.
Participate in professional organizations that provide regulatory updates and interpretation. Industry associations often offer valuable guidance about implementing new requirements.
Attend educational programs focused on regulatory compliance and quality improvement. Invest in training that helps you understand what to do and why requirements exist.
Subscribe to official updates from CMS and other regulatory bodies. Get information directly from the source rather than relying on secondhand interpretation.
Build relationships with consultants who specialize in hospice regulation. Expert guidance can help you navigate complex requirements more effectively.
Create internal systems for tracking regulatory changes and their impact on your operations. Document your compliance efforts to demonstrate good faith implementation.
Audit preparation should be ongoing rather than something you do when surveyors are coming. Continuous audit readiness ensures that your quality improvement efforts align with regulatory expectations.
Key audit preparation strategies:
Regular internal audits that identify potential issues before external reviewers arrive. Use the same standards that surveyors will use to evaluate your performance.
Documentation review that ensures your records tell a complete story about the excellent care you provide. Clean up documentation systems that may be confusing or incomplete.
Staff training on regulatory requirements and proper documentation. Everyone should understand their role in maintaining compliance.
Mock surveys that simulate the actual audit experience. Practice makes perfect and helps staff feel more confident when real surveyors arrive.
Corrective action protocols that address issues quickly and thoroughly. Demonstrate your commitment to continuous improvement.
| Audit Area | Preparation Strategy | Key Documentation | Staff Responsibility |
|---|---|---|---|
| Patient Rights | Policy review, staff training | Consent forms, care plans | All staff understand and implement |
| Care Planning | Documentation review, coordination | Comprehensive care plans, updates | Nurses, social workers, physicians |
| Symptom Management | Outcome tracking, medication review | Assessment notes, interventions | Clinical staff, pharmacists |
| Quality Assurance | Data analysis, improvement plans | QAPI reports, corrective actions | Leadership, quality team |
| Staff Qualifications | Training records, competency validation | Personnel files, education records | HR, clinical managers |
Risk mitigation in hospice care focuses on preventing problems that could harm patients, families, or your organization. Effective risk mitigation supports HCI improvement by creating stable systems consistently delivering excellent care.
Key risk areas and mitigation strategies:
Clinical Risk
Documentation Risk
Compliance Risk
Operational Risk
The most effective risk mitigation strategies are proactive rather than reactive. Identify potential problems before they occur and create systems that prevent them.
Remember that risk mitigation should support your mission rather than hinder it. The goal is to create safe, sustainable systems that enable excellent patient care while protecting your organization’s ability to serve families in the future.
Overcoming challenges is part of the journey toward HCI excellence. When you approach obstacles with creativity, persistence, and focus on patient benefit, you’ll find solutions that solve immediate problems and strengthen your entire organization. Every challenge you overcome makes you more capable of providing the excellent comfort care that patients and families deserve.
The path to HCI excellence isn’t always easy, but it’s always worthwhile. Your commitment to overcoming challenges demonstrates your dedication to the sacred mission of hospice care—providing comfort, dignity, and peace during life’s most important transition.
Achieving perfect HCI scores doesn’t happen overnight. It requires a thoughtful, systematic approach that builds excellence step by step. Think of this journey as building a house—you need a solid foundation before you can add the walls, and you need walls before you can put them on the roof. Each phase builds on the previous one, creating sustainable excellence that serves patients and families for years to come.
Your infrastructure is the backbone that supports all your HCI improvement efforts. Even the best intentions will struggle to create lasting change without strong systems.
Infrastructure development begins with an honest assessment of your current systems. What’s working well? What creates frustration for staff? What makes it harder to provide excellent comfort care? This isn’t about blame—it’s about understanding what needs to be built or improved.
Key infrastructure elements include:
Technology infrastructure should make care easier, not harder. If your current systems create barriers to excellent care, this is the time to address them. Simple, user-friendly systems that support your team’s work will have more impact than complex solutions that require extensive training.
Don’t try to fix everything at once. Start with the infrastructure elements that create the most frustration or have the biggest impact on patient care. Build success gradually rather than overwhelming your team with too many changes.
Remember that infrastructure includes your policies and procedures. These written guides should be clear, practical, and focused on supporting excellent comfort care rather than just meeting regulatory requirements.
Your team is your most valuable asset in achieving HCI excellence. Team preparation ensures that everyone understands their role, has the necessary skills, and feels supported in their efforts to provide exceptional care.
Team preparation starts with clear communication about your HCI improvement goals and why they matter. Help your team understand that higher HCI scores mean better patient comfort and more peaceful deaths for the families you serve.
Essential team preparation activities:
Team preparation should be personalized to each individual’s experience level, learning style, and professional goals. New staff need different preparation than experienced team members who are adapting to new approaches.
Build confidence through gradual skill development. Start with basic competencies and gradually add more complex skills as team members demonstrate readiness. Success breeds success—help your team experience wins early in the process.
Create learning partnerships where experienced staff mentor newer team members. This not only accelerates learning but also builds the collaborative culture that’s essential for HCI excellence.
| Team Role | Preparation Focus | Key Skills | Support Needed |
|---|---|---|---|
| Clinical Staff | Assessment and intervention skills | Symptom management, communication | Ongoing education, mentorship |
| Support Staff | Care coordination and documentation | Organization, attention to detail | Training, clear procedures |
| Leadership | System oversight and improvement | Data analysis, team development | Resources, authority to act |
| Specialists | Expertise in specific areas | Advanced clinical knowledge | Collaboration tools, referral systems |
Standardized processes ensure consistent excellence regardless of which team member is providing care. This doesn’t mean rigid procedures that ignore individual patient needs—it means reliable approaches that can be adapted to each unique situation.
Process standardization focuses on the activities that most impact HCI scores. These are the moments where small variations in approach can create significant differences in patient outcomes.
Key processes to standardize:
Effective standardization balances consistency with flexibility. Your processes should provide clear guidance while allowing for professional judgment and individual patient needs.
Involve your team in developing standardized processes. The people who do the work daily often have the best ideas about what works and what doesn’t. Their input creates better processes and increases buy-in for implementation.
Document processes clearly and make them easily accessible. Use simple language, step-by-step formats, and visual aids when helpful. Good process documentation serves as both training material and reference guide.
Test your standardized processes with small groups before full implementation. This allows you to identify problems and adjust before rolling out to your entire team.
Pilot programs allow you to test your approach with a small group before full implementation. This reduces risk and allows you to learn from experience before committing all your resources.
Effective pilot programs start small with carefully selected participants who will likely succeed. Choose your most skilled and motivated team members for the initial pilot. Their success will create momentum for broader implementation.
Pilot program selection criteria:
Clear goals and measurement criteria help you evaluate whether your pilot program works. Know what success looks like before you begin, and track progress regularly.
Pilot programs should run long enough to capture meaningful data but not so long that lessons become stale. Typically, 30-60 days provide enough time to identify patterns and make initial adjustments.
Communication during pilot programs is crucial. Keep participants informed about progress, challenges, and adjustments. Regular check-ins help maintain momentum and identify problems early.
Feedback from pilot programs is gold for improving your approach before full implementation. This feedback comes from staff, patients, families, and data analysis.
Collect feedback systematically rather than relying on informal conversations. Use structured surveys, interviews, and focus groups to gather comprehensive information about what’s working and what needs improvement.
Key feedback areas to explore:
Analyze feedback objectively and look for patterns rather than isolated incidents. What problems show up repeatedly? What successes can be replicated? What adjustments would improve outcomes?
Feedback integration should be transparent. Share what you learned with your pilot participants and explain how their input will shape the final approach. This builds trust and demonstrates that you value their contributions.
Don’t be afraid to make significant changes based on feedback. The pilot program’s purpose is to learn and improve. Better to adjust now than to implement a flawed approach across your entire organization.
Continuous refinement means making ongoing improvements based on experience and changing needs. This isn’t about major overhauls—it’s about small, consistent adjustments that enhance effectiveness over time.
Refinement should be systematic rather than random. Establish regular review cycles where you assess progress, identify opportunities, and make targeted improvements.
Sources of refinement opportunities:
Refinement changes should be tested before full implementation, just like your initial pilot program. Small tests reduce risk and help you understand the full impact of changes.
Communication about refinements helps your team understand that improvement is an ongoing process. Celebrate the learning that comes from refinement rather than viewing it as failure to get things right initially.
Document refinements so you can track what works and what doesn’t. This creates institutional memory that benefits future improvement efforts.
| Refinement Area | Review Frequency | Key Indicators | Adjustment Criteria |
|---|---|---|---|
| Clinical Processes | Monthly | Patient outcomes, staff feedback | Consistent problems or opportunities |
| Documentation | Quarterly | Audit results, efficiency measures | Compliance issues or inefficiencies |
| Training Programs | Bi-annually | Competency assessments, performance | Skill gaps or knowledge deficits |
| Technology Systems | Annually | User satisfaction, functionality | Significant problems or new capabilities |
Performance fine-tuning is about perfecting your approach to achieve consistently excellent results. This phase focuses on small adjustments that create big improvements in patient comfort and HCI scores.
Fine-tuning requires detailed analysis of your performance data to identify patterns and opportunities. Look for subtle variations that might indicate opportunities for improvement.
Key areas for fine-tuning:
Fine-tuning should be data-driven rather than based on assumptions. Use specific metrics to guide your adjustments and measure their impact.
Understanding outliers is the best way to fine-tune care. Why do some patients have exceptional outcomes? What can you learn from these cases to improve care for everyone?
Fine-tuning is iterative. Make small changes, measure results, and adjust accordingly. This gradual approach prevents unintended consequences while steadily improving performance.
Best practice sharing spreads excellence throughout your organization and beyond. When you discover approaches that work particularly well, sharing them multiplies their impact.
Internal best practice sharing helps your entire team learn from successes. Create systematic ways for staff to share what works and learn from each other’s experiences.
Effective sharing mechanisms:
External best practice sharing contributes to the broader hospice community while building your agency’s reputation for excellence. Consider sharing your successes at conferences, in publications, or through professional networks.
Best practice sharing should be specific and actionable. General statements about doing better are less helpful than detailed descriptions of what worked, why it worked, and how others can replicate it.
Create a culture where sharing is valued and rewarded. Some staff may be hesitant to share their successes. Encourage and support those who are willing to help others learn.
Sustainability planning ensures your HCI improvements last beyond the initial implementation phase. This requires building systems and a culture that automatically maintain excellence.
Sustainable systems don’t depend on individual heroes. They create consistent excellence regardless of which staff members are involved. Build your systems to support rather than rely on exceptional individuals.
Key sustainability elements:
Leadership commitment is essential for sustainability. New leaders must understand and support the systems that create HCI excellence.
Sustainability planning should anticipate challenges like staff turnover, regulatory changes, and resource constraints. Build flexibility into your systems so they can adapt to changing circumstances.
Culture change is the ultimate sustainability strategy. When excellent care becomes “how we do things here,” it persists through all kinds of changes. Focus on creating a culture where HCI excellence is the natural result of your team’s commitment to comfort care.
| Sustainability Factor | Risk Level | Mitigation Strategy | Success Indicator |
|---|---|---|---|
| Staff Turnover | High | Comprehensive training, clear procedures | New staff achieve competency quickly |
| Leadership Changes | Medium | Documented systems, succession planning | Consistent performance across leadership transitions |
| Resource Constraints | Medium | Efficient processes, creative solutions | Maintained quality despite limitations |
| Regulatory Changes | Low | Flexible systems, ongoing education | Smooth adaptation to new requirements |
Remember that the road to 10/10 is a journey, not a destination. Each phase builds on the previous one to create sustainable excellence that serves patients and families for years to come. The systematic approach ensures that your improvements are lasting and meaningful rather than temporary or superficial.
Your commitment to this systematic approach honors the trust that patients and families place in your care. Every step you take toward HCI excellence is a step toward fulfilling hospice’s sacred mission of providing comfort, dignity, and peace during life’s most important transition.
The road may be challenging, but it’s also deeply rewarding. Your dedication to systematic excellence makes a real difference in the lives of the patients and families you serve, creating a legacy of compassionate care that extends far beyond any single metric or score.
While this article draws inspiration from Jose Escobar’s insightful work “Are You Missing the 10 Moments That Matter Most in Hospice?”, the content, interpretations, and recommendations presented here are from the author of CompassionCrossing.info. We sincerely appreciate Jose’s innovative contributions to hospice care excellence and his commitment to improving patient outcomes through systematic approaches. His Polaris 10/10 HCI Execution Framework has provided valuable insights that have influenced our understanding of what creates truly exceptional hospice care.
The journey to HCI excellence isn’t about achieving perfect scores for their own sake—it’s about creating systems that consistently deliver the comfort, dignity, and peace that every patient and family deserves during life’s most sacred transition.
The ten moments that matter most represent critical touchpoints where your actions directly impact both patient comfort and HCI scores. These moments aren’t random opportunities—they’re systematic intervention points where excellence significantly benefits the families you serve.
Key principles that guide HCI excellence:
The most important insight from this framework is that HCI excellence and exceptional patient care aren’t separate goals—they’re the same goal. When you systematically execute excellence during the ten moments that matter most, you simultaneously improve patient comfort and achieve higher HCI scores.
Implementation requires patience and persistence. The three-phase approach—foundation building, implementation, and optimization—ensures that improvements are sustainable rather than temporary. Each phase builds essential capabilities that support long-term success.
Success is measured not just by numbers but by the peace of mind that families experience, the dignity that patients maintain, and the professional satisfaction that comes from knowing you’ve provided excellent care during humanity’s most important transition.
The time for action is now. Every day that passes without systematic improvement is a missed opportunity to provide better care for the patients and families who trust you with their most vulnerable moments.
For Hospice Executives:
Your leadership sets the tone for everything that follows. Commit to providing the resources, support, and vision necessary for HCI excellence. This isn’t just about allocating budget—it’s about creating a culture where excellence is expected, supported, and celebrated.
Start by honestly assessing your current performance. Where are your greatest opportunities for improvement? What barriers prevent your team from providing excellent care? Use this information to create a strategic plan that addresses root causes rather than symptoms.
Invest in your team’s development. Your staff wants to provide excellent care, but they need the tools, training, and support to make that excellence consistent and sustainable. Your investment in their growth directly benefits the patients and families you serve.
For Clinical Managers:
You’re the bridge between vision and reality. Your role is to create systems and processes that make excellence achievable for your frontline staff.
Focus on the ten moments that matter most. Help your team understand these critical touchpoints and develop the skills needed to execute them with precision and compassion. Create supportive environments where staff feel confident and capable.
Use data to guide improvement efforts. Regular monitoring of HCI scores, patient outcomes, and staff feedback helps you identify what’s working and what needs adjustment. Let evidence guide your decisions rather than assumptions.
For Direct Care Staff:
Your daily interactions with patients and families create the experiences that define hospice care. Every assessment, every intervention, every conversation is an opportunity to demonstrate excellence.
Embrace the ten moments framework as a tool for organizing your care rather than an additional burden. These moments represent the activities that make the biggest difference in patient comfort and family satisfaction.
Continue learning and growing. The most effective hospice professionals are those who remain curious, open to new approaches, and committed to continuous improvement. Your professional development directly benefits the families you serve.
Remember that excellence is a team effort. Share your successes, learn from your colleagues, and contribute to a culture where everyone supports each other in providing exceptional care.
Imagine a future where every hospice patient receives truly exceptional care—where pain is managed effectively, families feel supported and prepared, and death occurs with dignity and peace. This isn’t just a dream—it’s an achievable goal when hospice agencies commit to systematic excellence.
The future of hospice care excellence is characterized by:
Predictable Excellence: Agencies that use systematic approaches like the Polaris 10/10 Framework consistently achieve HCI scores of 9-10 because they’ve built systems that naturally produce excellent outcomes.
Empowered Staff: Hospice professionals who have the tools, training, and support they need to provide exceptional care find deep satisfaction in their work. Staff turnover decreases while job satisfaction and professional pride increase.
Confident Families: Patients and families served by excellent hospice agencies feel more prepared, supported, and peaceful during the dying process. They trust their hospice team to provide skilled, compassionate care that honors their values and preferences.
Sustainable Operations: Agencies that achieve HCI excellence also achieve operational sustainability. Quality and financial performance go hand in hand when systems are designed for excellence and efficiency.
Industry Leadership: The hospice industry becomes recognized as a model for healthcare excellence, demonstrating that systematic quality improvement approaches can create better outcomes and greater stakeholder satisfaction.
This vision requires collective commitment from every hospice professional, from executives to frontline staff. Each person who dedicates themselves to systematic excellence contributes to a future where hospice care consistently reflects the best of healthcare.
The families you serve deserve nothing less than your best. They come to hospice during their most vulnerable moments, trusting you to provide skilled, compassionate care that honors their loved one’s life and supports their transition. Your commitment to HCI excellence is ultimately a commitment to honoring that trust.
The journey toward HCI excellence is challenging but deeply rewarding. Every improvement you make, every system you strengthen, and every moment you execute with precision and compassion creates a ripple effect that extends far beyond any single metric.
Your dedication to this work matters. In a world that often feels chaotic and uncertain, hospice professionals provide something precious—the promise that no one has to face death alone, that suffering can be minimized, and that life’s final chapter can be written with dignity and peace.
Together, we can create a future where HCI excellence is the standard rather than the exception, where every patient receives the comfort care they deserve, and where the sacred work of hospice care is performed with the systematic excellence that honors both the living and the dying.
The road to 10/10 isn’t just about achieving perfect scores—it’s about creating perfect moments of comfort, dignity, and peace for every family you have the privilege to serve. That’s a vision worth pursuing with all the skill, compassion, and determination you can bring to this sacred work.
Are You Missing the 10 Moments That Matter Most in Hospice? by Jose Escobar
Jose Escobar of the Polaris Group LinkedIn Profile
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Holistic Nurse: Skills for Excellence book series
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.