Understanding Palliative Care: A Guide to Common Questions and Answers
Published on February 7, 2025
Updated on February 4, 2025
Published on February 7, 2025
Updated on February 4, 2025
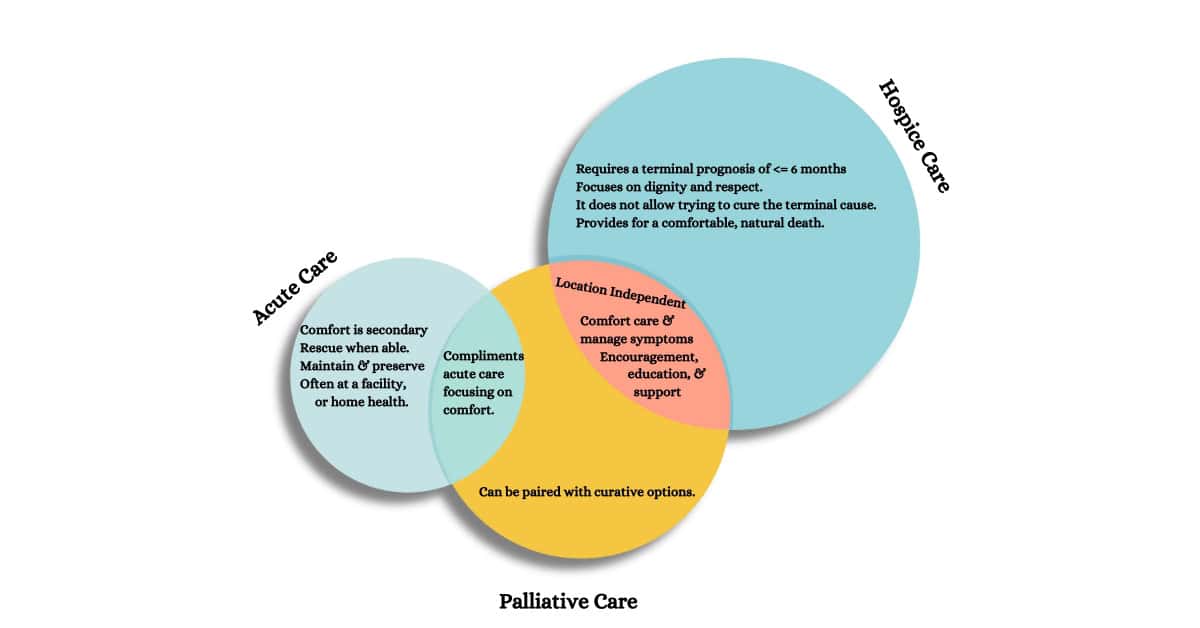
Table of Contents
When you or a loved one is facing a severe illness, every moment is precious, especially those spent with family and friends. Palliative care is a specialized form of medical care that focuses on relieving the symptoms and stress of a severe illness. Its goal is to improve the patient’s and family’s quality of life.
Palliative care is provided by a specially trained team of doctors, nurses, and other specialists who work with a patient’s other doctors to offer extra support. It is appropriate at any age and stage of a severe illness and can be provided alongside curative treatment. The care is tailored to meet each person’s needs, ensuring they receive comprehensive physical, emotional, and spiritual support.
Understanding palliative care is crucial because it empowers you and your loved ones to make informed decisions about your healthcare. Knowing what palliative care involves can help you advocate for the best possible care, ensuring that the patient’s wishes are respected and their needs are met. It’s about living as well as possible for as long as possible.
Palliative care is a particular health care for individuals with serious illnesses. It’s focused on providing relief from symptoms and stress. The goal is to improve the quality of life for both the patient and their loved ones. It’s not just about treating the illness; it’s about caring for the whole person. This means addressing physical discomfort, emotional challenges, and spiritual questions that may arise. It’s a team approach involving doctors, nurses, social workers, and other specialists who work together to provide support tailored to the individual’s needs.
Palliative and hospice care share the same core values: comfort and support. However, they differ in when and how they are provided. Palliative care can begin at diagnosis and at the same time as treatment. Hospice care starts after treatment of the disease is stopped and when it is clear that the person is not going to survive the illness. Think of palliative care as a support system at any stage of a severe illness, while hospice care provides comfort during the final phase of life.
Palliative care is a resource for anyone living with a severe illness, such as heart failure, chronic obstructive pulmonary disease, cancer, dementia, Parkinson’s disease, and many others. It’s not just for those at the end of their lives. If you’re experiencing a lot of pain, stress, or other severe symptoms due to your illness, palliative care can help. It’s about enhancing your quality of life and supporting you through your medical journey.
Accessing palliative care services starts with a conversation with your doctor. They can refer you to a palliative care specialist. Many hospitals have palliative care teams; services can also be found in outpatient clinics and sometimes at home. Insurance plans, including Medicare and Medicaid, often cover palliative care services. It’s also a good idea to check with your insurance provider to understand the specifics of your coverage.
Palliative care is a comprehensive service that addresses various needs of patients with serious illnesses. It includes:
Yes, palliative care can often be received at home. This allows patients to stay in a familiar and comfortable environment surrounded by their loved ones. Home-based palliative care services can include regular professional visits, medication management, and coordination with the patient’s healthcare team to ensure that care plans are followed and symptoms are effectively managed.
A palliative care team is like a group of caring friends, each with unique skills to help you through a tough time. This team usually includes:
Your family is an essential part of your care team. They know you best and can help the medical team understand your wishes. They can also help with daily care and make sure you’re comfortable. In palliative care, we believe that supporting your family is as important as supporting you. They receive guidance on caring for you and emotional support to help them through this journey with you.
Pain can be a significant concern for patients with serious illnesses. In palliative care, managing pain is a priority because it affects every part of your life. The care team works to understand the cause of your pain and provide treatments that can include:
The goal is to control pain so that you can be as comfortable and active as possible. Your care team will listen to you and adjust treatments as needed because your comfort matters most.
Palliative care also focuses on symptoms other than pain, such as:
Your palliative care team understands that these symptoms can be just as troubling as pain, and they’re here to help you find relief and maintain your quality of life.
Dealing with a severe illness can be emotionally taxing, not just for the patient but also for their loved ones. Palliative care provides a comforting presence, offering emotional support to help ease anxiety, fear, and depression that may come with illness. This support includes:
The goal is to ensure that no one feels alone in this journey and that emotional well-being is nurtured alongside physical health.
Spirituality can provide comfort and strength for many facing severe illness. In palliative care, spiritual care is tailored to each person’s beliefs and may include:
Spiritual care in palliative care is about respecting each person’s spiritual path and providing support that aligns with their values and beliefs.
Navigating insurance coverage for palliative care can seem daunting, but understanding your policy can provide peace of mind. Most insurance plans, including Medicare and Medicaid, cover palliative care services. This coverage typically includes:
Talking to your insurance provider about what is covered under your plan is essential. They can explain how benefits are applied and what costs you might expect. Some questions to ask might include:
Advance directives are legal documents that allow you to outline your preferences for medical treatment in case you cannot communicate your decisions. They are a crucial part of planning for palliative care. There are two main types:
Creating these documents involves thoughtful consideration and discussions with your loved ones and healthcare providers. They ensure your wishes are known and respected and guide your family and doctors.
Cancer affects not just the body but also the heart and mind. Palliative care for cancer patients is personalized to address their unique challenges. It includes:
Cancer palliative care is more than managing symptoms; it’s about supporting patients and families through one of life’s toughest challenges.
Palliative care isn’t just for cancer. It’s also for those with chronic, progressive illnesses like heart disease, lung disease, Alzheimer’s, and many others. For these patients, palliative care focuses on:
Whether it’s cancer or another serious illness, palliative care is about adding life to days, even when days cannot be added to life.
In today’s world, technology brings us closer, even in healthcare. Telemedicine allows patients receiving palliative care to connect with their healthcare team from their homes. This can be exceptionally comforting when travel to a hospital or clinic is difficult. Symptoms can be managed effectively through video calls, phone chats, and remote monitoring. It means:
Remote care options ensure that you’re not alone in managing your illness. Help is just a call or click away.
Palliative care isn’t just about comfort; it’s also about hope. Innovative treatments, such as new medications and therapies, are part of palliative care. These might include:
Innovative treatments in palliative care aim to improve your quality of life, offering new possibilities for comfort and care.
The journey through a severe illness is filled with many steps, and one of the most significant is the transition from palliative care to hospice. This transition happens when treatment is no longer focused on curing the illness but on providing comfort and the highest quality of life possible. Here’s what this change involves:
You don’t have to navigate the path of serious illness alone. There are many resources available to provide support:
Remember, seeking support is a sign of strength. It means you’re taking an active role in your care or caring for your loved one.
Palliative care is a beacon of comfort and support during the stormy times of a severe illness. It’s about more than just managing symptoms; it’s about caring for the whole person—body, mind, and spirit. This type of care brings together a team of compassionate professionals dedicated to easing pain, soothing stress, and providing the best possible quality of life for patients and their families.
Every person’s journey with illness is unique, and so is their experience with palliative care. That’s why it’s so important to seek personalized advice from healthcare professionals who understand your situation. They can offer tailored guidance that respects your wishes and addresses your needs. Don’t hesitate to ask questions, share your concerns, and express your preferences. Remember, you are the most essential care team member; your voice matters.
In closing, palliative care is a testament to the power of holistic, patient-centered healthcare. It reminds us that even in the most challenging times, there are people ready to help and support us every step of the way. So reach out, get the personalized advice you deserve, and take comfort in knowing that palliative care is there to walk this path with you.
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death