-

A Complete Guide to Hiring Caregivers for Terminally Ill Patients
Discover the essentials of hiring caregivers for terminally ill patients. This guide covers caregiver qualifications, assessing understanding of terminal care, and practical hiring tips. -
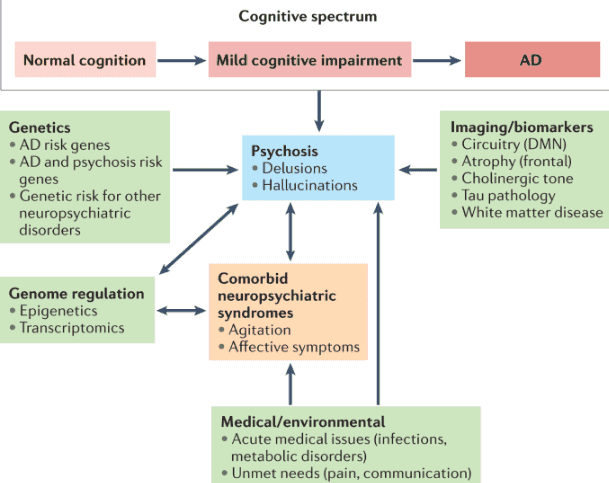
A Comprehensive Guide to Dementia-Induced Psychosis for Hospice Care Providers
This guide provides hospice nurses, caregivers, and family members with essential information on dementia-induced psychosis, including its signs, symptoms, differentiation from other conditions, and effective management strategies. -

A Comprehensive Guide to Diabetes Management for Loved Ones with Dementia
Discover essential strategies for managing diabetes in loved ones with dementia. This comprehensive guide covers blood sugar monitoring, medication administration, diet management, and recognizing emergencies, empowering caregivers to provide optimal care. -

A Comprehensive Guide to Diagnosing Dementia and Providing Compassionate Care
Dementia is a complex condition affecting millions worldwide. Diagnosing dementia requires the expertise of medical professionals specializing in cognitive disorders. By guiding families and caregivers through the diagnostic process, you can empower them. In this article, we’ll explore the steps to find the right specialist for a dementia diagnosis and how families can prepare for the crucial doctor visit. -

A Summary Review of the Twelve Known Types of Dementia
This article summarizes the twelve known types of dementia, which are the most common and well-studied forms of this condition. You will learn about the signs and symptoms of each type, how they are diagnosed, what causes them, and how they are treated. This article is intended for family members and caregivers of people with dementia who may want to understand more about the condition and how to support their loved ones. -

Abdominal Aortic Aneurysm: A Life-Threatening Condition for Hospice Patients
The purpose of this article is to provide you with some information and guidance about AAAs and how they can be managed in hospice patients. -

Adrenal Insufficiency Crisis Management for Terminally Ill Patients
Discover essential strategies for managing adrenal insufficiency crises in terminally ill patients. Learn about symptoms, risk factors, and crucial interventions to ensure patient comfort and safety. This guide provides valuable insights for hospice nurses and caregivers in this critical condition. -
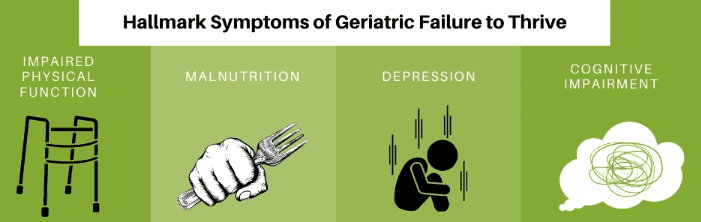
Adult Failure to Thrive: A Guide for Caregivers
Discover essential insights into Adult Failure to Thrive—a condition affecting older adults. Learn why early recognition and compassionate care are crucial for improving quality of life. -
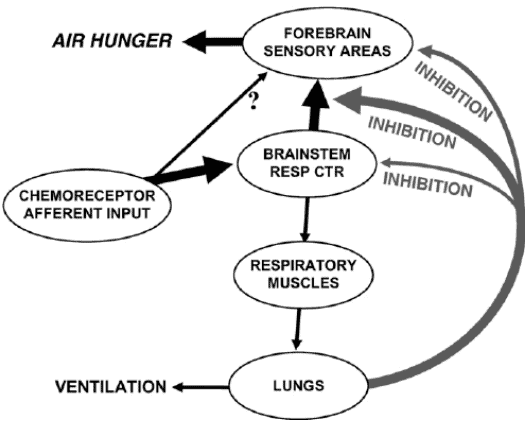
Air hunger management at end-of-life
I can count the times I’ve run into air hunger at the end of life as a visiting RN Case Manager for going on five years on one hand. Over the years, I’ve managed patients with pulmonary fibrosis, lung cancers (diverse types), breast cancer, COPD, congestive heart failure, B-cell lymphoma, leukemia, and other diseases that can impact one person’s ability to breathe correctly. Air hunger is rare in my firsthand experiences, but it can happen. Air hunger often sounds like the person is gasping for breath without regard to the actual respiratory rate (how fast they are breathing); it can also sound like stridor (YouTube videos below where you can hear the difference). -

Alcoholic Cirrhosis of the Liver with Ascites: A Guide for Families
Discover crucial information about alcoholic cirrhosis of the liver with ascites in this comprehensive guide for caregivers and family members. Learn about symptoms, diagnosis, treatment options, and practical tips for providing care. Understand what to expect in the terminal stage and find resources for emotional support during this challenging journey. -
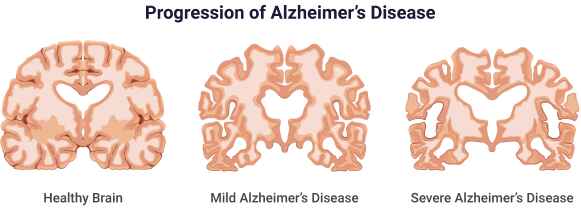
Alzheimer’s Disease: Understanding the Most Prevalent Form of Dementia
Delve into the complexities of Alzheimer’s disease, the most common form of dementia. This article examines its causes, symptoms, diagnosis, and treatment options while discussing the challenges patients and caregivers face. Learn about ongoing research and potential breakthroughs in the fight against this devastating neurological disorder. -
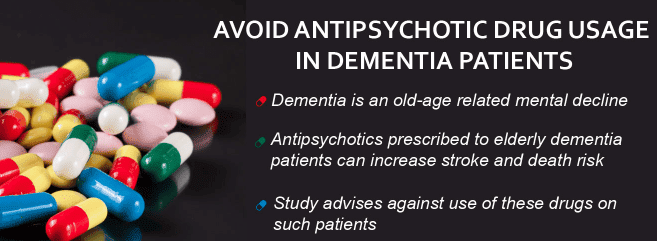
Antipsychotics & Dementia Risk: A Critical Analysis
Unveiling the connection between antipsychotic drugs and dementia, this article delves into how these medications may elevate the risk or exacerbate symptoms. It provides a thorough examination of current research, expert opinions, and alternative approaches to managing dementia. -
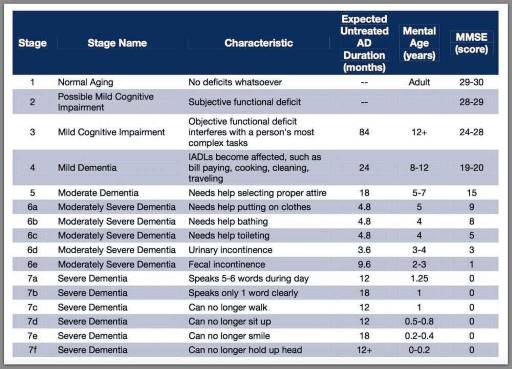
Assessing Patients on the FAST Scale: A Guide for Nurses
As a nurse who has cared for many terminally ill individuals with Alzheimer’s disease over the years, I understand the importance of accurately assessing their functional decline using the Functional Assessment Staging Tool (FAST). The FAST scale provides valuable information about the progression of Alzheimer’s disease and helps guide appropriate care planning for patients and their families. In this guide, I will walk you through the process of assessing patients on the FAST scale, starting from stage 1 and discussing when to stop reading the scale for determination. I will also provide three examples of patients at various stages of the FAST scale. -
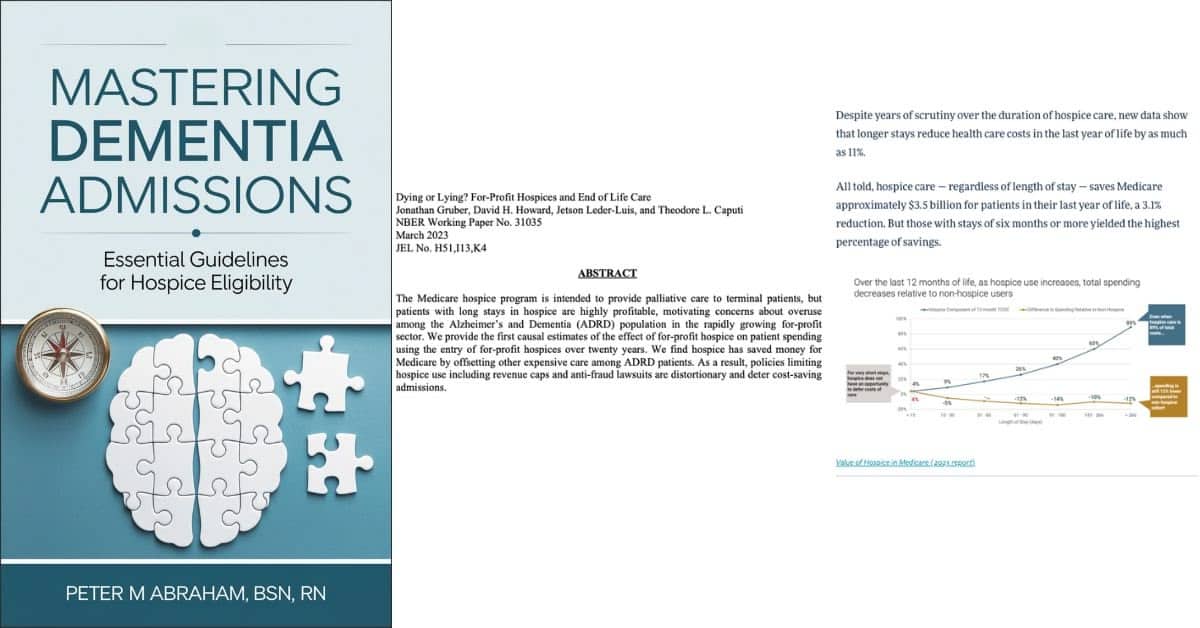
Balancing Patient Care and Compliance: The Impact of Extended Hospice Care for Dementia Patients
Explore how extended hospice care for dementia patients benefits families and saves Medicare money despite regulatory challenges around six-month prognosis rules. -

Best Practices for Approaching Combative Dementia Patients
Dementia is a progressive brain disorder that affects a person’s cognitive abilities, memory, and behavior. In the later stages of the disease, some patients can become combative and aggressive, making it difficult for caregivers to provide the necessary care. As a hospice nurse, it’s important to know how to approach and manage combative dementia patients to ensure their comfort and safety. Here are some best practices to consider: