How Different Types of Illnesses Affect Our Lives and Deaths: A Summary of a Research Paper by Joanne Lynn and Colleagues
Published on September 25, 2024
Updated on December 3, 2025
Published on September 25, 2024
Updated on December 3, 2025
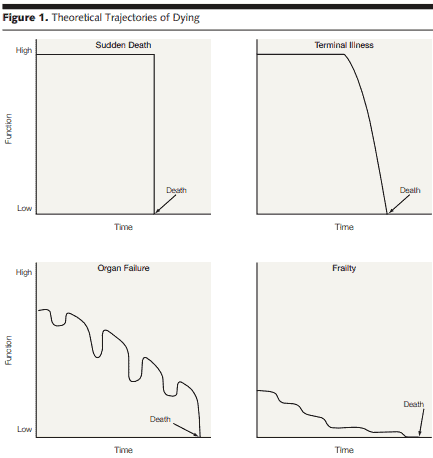
Table of Contents
Have you ever wondered how different illnesses affect our lives and deaths? How do we cope with the uncertainty and unpredictability of our health? How do we plan for our future and make the best decisions for ourselves and our loved ones?
These are some of the questions a research paper by Joanne Lynn and colleagues tried to answer. The paper, published in the Journal of the JAMA in May 2003, examined the four common types of illness trajectories that most people experience before they die. These trajectories are:
The paper analyzed the characteristics, prevalence, and outcomes of these trajectories, and their implications for health care and social support. It also proposed strategies and recommendations to improve the quality of life and care for people with diverse trajectories.
The main findings of the paper were:
In this article, we will summarize and discuss the paper’s main points and findings, and explore how they relate to our lives and deaths. We will also provide practical and actionable suggestions for coping with and planning for your and your loved ones’ trajectories. We aim to help you understand the different illness trajectories, how they affect our lives and deaths, and how we can prepare for them.
Sudden death is a term that describes the sudden and unexpected loss of life due to a problem in the heart or the brain. It can happen to anyone, even those who seem healthy and have no known medical conditions. Sudden death can be caused by various factors, such as:
Sudden death is a serious public health issue that affects millions of people worldwide. According to the World Health Organization, about 17.9 million people die each year from cardiovascular diseases, which are the leading cause of sudden death. In the United States, about 325,000 people die each year from sudden cardiac death, which accounts for about half of all heart disease deaths. Sudden death can also occur in young people, especially athletes. Some estimates suggest that about 1 in 50,000 to 1 in 80,000 young athletes die of sudden cardiac death each year.
Sudden death can be prevented or reduced by identifying and managing the risk factors that can trigger or worsen the underlying conditions. Some of these risk factors include:
Some of the prevention strategies that can help lower the risk of sudden death include:
Sudden death can have devastating consequences for individuals, families, and society. It can cause emotional trauma, grief, and loss for the loved ones of the deceased. It can also have economic and social impacts, such as loss of income, reduced productivity, and reduced contributions to the community. Sudden death can also raise legal and ethical issues, such as the need for an autopsy, organ donation, and inheritance. Therefore, it is important to raise awareness and education about the causes, risk factors, and prevention strategies of sudden death and to provide support and resources for the survivors and the bereaved.
Cancer death is a term that describes the loss of life due to cancer, which is a disease that causes abnormal cells to grow and spread in the body. Cancer cells can form tumors that interfere with the normal functioning of organs and tissues. Cancer death occurs when the cancer becomes too advanced or aggressive to be controlled by any available treatments or when the treatments cause too much harm or side effects to the patient.
Cancer is a leading cause of death worldwide, accounting for nearly 10 million deaths in 2020. The most common types of cancer that cause death are lung, colorectal, breast, prostate, stomach, liver, and pancreatic cancer. The risk of developing and dying from cancer depends on many factors, such as age, sex, race, genetics, lifestyle, and environmental exposure. Some of these factors can be modified or prevented, such as smoking, drinking, obesity, and sun exposure, while others cannot, such as family history and aging.
Cancer treatment options vary depending on the type, stage, and location of the cancer, as well as the patient’s preferences and overall health. Some of the common treatment options include surgery, chemotherapy, radiation therapy, immunotherapy, targeted therapy, and hormone therapy. These treatments aim to remove, shrink, or stop the growth of cancer cells, relieve the symptoms, and improve the patient’s quality of life. However, not all cancers can be cured or controlled by these treatments, and some cancers may become resistant or recur after treatment. In some cases, the benefits of treatment may not outweigh the risks or side effects, and the patient may decide to stop or refuse treatment.
Cancer death can have devastating effects on individuals, families, and society. It can cause physical, emotional, social, and spiritual suffering for the patient and their loved ones. It can also have economic and legal impacts, such as loss of income and productivity, insurance coverage, and the need for advance care planning, wills, and funeral arrangements. It is important to provide support and resources for the patients and their families facing cancer death and to respect their wishes and dignity.
Death from organ failure is a term that describes the loss of life due to chronic diseases that affect one or more of the vital organs in the body. Vital organs are essential for survival, such as the heart, lungs, kidneys, liver, and brain. When these organs are damaged or diseased, they cannot perform their normal functions, and the body’s ability to maintain homeostasis (a stable internal environment) is compromised. Death from organ failure occurs when the organ damage is so severe that it cannot be reversed or treated, and the body’s systems fail.
Death from organ failure is a common cause of death worldwide, especially among older people and people with multiple chronic conditions. According to the Centers for Disease Control and Prevention (CDC), the leading causes of death in the United States in 2021 were heart disease, cancer, COVID-19, unintentional injuries, stroke, chronic lower respiratory diseases, Alzheimer’s disease, diabetes, chronic liver disease and cirrhosis, and kidney disease. All of these conditions can lead to organ failure and death if not diagnosed and appropriately managed.
The risk factors for developing and dying from organ failure vary depending on the type and cause of the organ damage. Some of the common risk factors include:
The management strategies for preventing and treating organ failure depend on the type and severity of the organ damage, the patient’s preferences, and overall health. Some of the common management strategies include:
Death from organ failure can have profound impacts on individuals, families, and society. It can cause physical, emotional, social, and spiritual distress for the patients and their loved ones. It can also have economic and legal implications, such as loss of income and productivity, insurance coverage, and the need for advance directives, wills, and funeral arrangements. It is important to provide support and resources for the patients and their families facing organ failure and death, and to respect their wishes and dignity.
Frailty is a term that describes a condition that affects some older people, making them more vulnerable and less resilient to stressors. Stressors such as illness, injury, infection, or emotional distress can challenge or harm the body or the mind. Frailty is not a normal part of aging but a complex and multidimensional syndrome that involves physical, psychological, and social aspects of health. Frailty can affect a person’s ability to cope with daily activities, recover from illness or injury, and maintain their independence and well-being.
Frailty is a widespread problem among older people, especially those who are very old or have multiple chronic diseases. According to some studies, about 10% of people over 65 have frailty, increasing to 25% and 50% for those over 85. However, the exact prevalence of frailty may vary depending on how it is defined and measured. There are several ways to assess frailty, including questionnaires, physical tests, and clinical criteria. Some of the common signs and symptoms of frailty include:
Frailty can be caused or worsened by various factors, some of which can be modified or prevented and some of which cannot. Some of the common risk factors for frailty include:
Frailty can be prevented, delayed, or reversed by adopting healthy and active lifestyles and receiving appropriate and timely medical and social care. Some of the common intervention approaches for frailty include:
Frailty can have profound consequences for individuals, families, and society. It can cause physical, emotional, social, and spiritual distress for patients and their loved ones. It can also have economic and legal implications, such as loss of income, reduced productivity, insurance coverage, independence, and the need for advance directives, wills, and funeral arrangements. It is important to provide support and resources for patients and their families facing frailty and to respect their wishes and dignity.
The research paper by Joanne Lynn and colleagues provides valuable insights into the different illness trajectories most people experience before they die. The paper’s analysis of sudden death, cancer death, death from organ failure, and frailty sheds light on the characteristics, prevalence, and outcomes of these trajectories, as well as their implications for health care and social support. The paper’s main findings underscore the need for different approaches and interventions to optimize the well-being and dignity of individuals and their families and the challenges and opportunities these trajectories present for the healthcare system and society. The implications of this research are profound, as it highlights the diverse impacts of these illness trajectories on the psychological, social, and spiritual aspects of life and death. It also emphasizes the importance of tailored care and support to address the unique needs of individuals facing these trajectories. As a hospice registered nurse case manager, it is crucial to recognize and understand these trajectories to provide compassionate and person-centered care to terminally ill patients and their families. In conclusion, this research paper is valuable for healthcare professionals, caregivers, and individuals facing these illness trajectories. It underscores the significance of proactive planning, support, and education to navigate the complexities of these trajectories and ensure the best possible quality of life for patients and their loved ones. By acknowledging and addressing the distinct challenges posed by each trajectory, we can work towards enhancing the end-of-life journey for individuals and families, aligning with the principles of empathy and compassion that are fundamental to hospice care.
Patterns of Functional Decline at the End of Life
Time Course of Dying – Fundamentals – Merck Manuals
Latest Statistics | Sudden Cardiac Arrest Foundation
Sudden death in young people: Heart problems often blamed
Sudden death syndrome: Causes, prevention, FAQ, and more
World health Organization – Cancer
Choices for Care with Advanced Cancer
FastStats – Leading Causes of Death
Mortality in the United States, 2021
Kidney Disease Statistics for the United States
Organ Failure: Signs & Symptoms, Causes, Stages, Treatment
Multiple Organ Dysfunction Syndrome: Causes, Treatment, Prevention
Frailty: Evaluation and Management
Interventions for Frailty and Preventing the Development of Frailty
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death