Educating Facility Staff on What Matters for Terminally Ill Patients
Published on July 21, 2023
Updated on July 6, 2024
Published on July 21, 2023
Updated on July 6, 2024
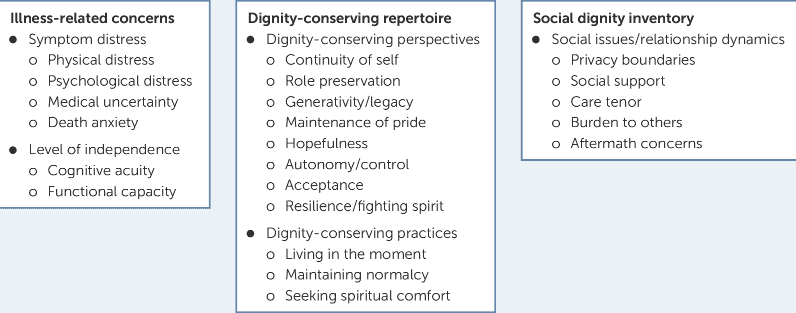
Table of Contents
As an experienced hospice nurse, I understand the importance of educating nursing home staff who may not be accustomed to caring for terminally ill patients. Hospice care is a specialized field that focuses on providing comfort, support, and dignity to individuals nearing the end of their lives. Here are the top five areas that hospice nurses should address when educating nursing home staff:
In hospice care, the emphasis shifts from constantly monitoring vital signs to prioritizing the comfort and quality of life of the terminally ill patient. It’s crucial to explain to nursing home staff that hospice care aims to manage symptoms, alleviate pain, and provide emotional support rather than pursuing curative treatments. By understanding this shift in focus, nursing home staff can better meet the needs of terminally ill patients.
I’ve witnessed the transformative impact of shifting the emphasis from constant monitoring to prioritizing the comfort and quality of life for terminally ill patients. When working with nursing home staff, it’s essential to communicate the purpose and goals of hospice care effectively. Here’s how I would explain it:
A. Shifting the Emphasis: Explain that in hospice care, the focus changes from pursuing curative treatments to providing symptom management, pain relief, and emotional support. The goal is to enhance the patient’s quality of life during their remaining time.
B. Educating on Symptom Management: Highlight the importance of effectively managing symptoms such as pain, shortness of breath (not based on SPO2), nausea, and anxiety. Discuss the various approaches and medications used in hospice care to alleviate these symptoms and enhance comfort.
C. Empathy and Understanding: I would begin by expressing empathy and understanding for the challenges nursing home staff often face when caring for terminally ill patients. I would acknowledge their dedication and the importance of their role in providing comfort and support.
D. Collaboration and Support: Emphasize that the hospice team works collaboratively with nursing home staff, sharing knowledge and expertise to optimize the patient’s care. Assure them that their input and observations are valued and considered in the care plan.
E. Psychosocial Support: Stress the significance of addressing the patient’s and their loved ones’ emotional and psychosocial needs. Explain how hospice provides counseling, support groups, and bereavement services to help patients and families navigate the challenges they may face.
By providing nursing home staff with this understanding and knowledge, they can better align their care practices with hospice’s goals and philosophy. We can create a compassionate and supportive environment for terminally ill patients.
One of hospice nurses’ critical responsibilities is managing symptoms and controlling pain for terminally ill patients. Educating nursing home staff about various strategies and interventions for symptom management, such as administering appropriate medications, positioning techniques, and non-pharmacological comfort measures, is essential. Guiding, assessing, and addressing common symptoms like pain, nausea, breathlessness (not always managed by external oxygen), and anxiety can significantly enhance the quality of care provided.
Pharmacological education needs to include PRN medications can be given at the same time as routine medications, removing the myth that PRN times and routine times are connected, that comfort medications do not euthanize or otherwise hasten the dying process, and that facility staff can cause significant harm to the patient by allowing their biases toward comfort medications interfere with the keeping the patient comfortable.
Terminally ill patients and their families often require emotional support and guidance during this challenging time. Hospice nurses are trained to provide psychosocial support, actively listen, and facilitate effective communication between patients, families, and the interdisciplinary care team. Educating nursing home staff on how to empathize, actively listen, and address the psychosocial needs of patients and their families is essential, fostering open and compassionate communication.
Hospice nurses are crucial in assisting patients and their families with end-of-life care planning and discussing advance directives. Educating nursing home staff about the importance of advance care planning, including discussions on goals of care and treatment options, and documenting patients’ wishes ensures that the care provided aligns with the patient’s preferences. It’s essential to emphasize respecting patient autonomy and involving families in these discussions.
Caring for terminally ill patients extends beyond their passing. Hospice nurses provide bereavement support and grief counseling to families, helping them navigate the grieving process. Educating nursing home staff on the importance of supporting families after a patient’s death, providing resources for grief counseling, and understanding the dynamics of grief can contribute to holistic and compassionate care.
Remember, hospice nurses have a wealth of experience and expertise in caring for terminally ill patients. By sharing our knowledge and skills with nursing home staff, we can enhance the care provided to those in need.
The education of nursing home staff on hospice care for terminally ill patients is crucial for ensuring the comfort, support, and dignity of individuals nearing the end of their lives. By focusing on critical areas such as shifting the emphasis from vital signs to comfort, effective symptom management, psychosocial support, end-of-life care planning, and bereavement support, hospice nurses can empower nursing home staff to align their care practices with the goals and philosophy of hospice. This collaboration can lead to the creation of a compassionate and supportive environment for terminally ill patients. The efficacy of hospice care in managing pain and symptoms, the importance of psychosocial support and communication skills, end-of-life care planning, and advance directives, as well as the provision of bereavement support and grief counseling, are all essential components of educating nursing home staff on what matters for terminally ill patients. By sharing their knowledge and skills, hospice nurses can enhance the overall care provided to those in need, ultimately contributing to a more compassionate and person-centered approach to end-of-life care.
The Nurse Advocate in End-of-Life Care
The Role of Hospice Care in the Nursing Home Setting
Hospice in the Nursing Home: Perspectives of Front-Line Nursing Home Staff
A Terminal Diagnosis: Strategies for Helping Patients and Their Loved Ones
The palliative care education needs of nursing home staff
Preparing for a Good Death: Topics to Cover with Hospice Patients and Their Families
Should dying patients be on oxygen?
Presentation: Death, Dying, and Comfort Medications in Hospice Care
Guide to Recognizing and Treating Common End of Life Symptoms
Pain Assessment in Hospitalized Older Adults With Dementia and Delirium
Pain Assessment in Dementia – International Association for the Study of Pain (IASP)
Pain Assessment in People with Dementia: AJN The American Journal of Nursing
Pain Assessment in Advanced Dementia Scale (PAINAD) – MDCalc
Uncontrolled Pain and Risk for Depression and Behavioral Symptoms in Residents With Dementia
Pain Assessment and Pharmacologic Management
Adult Nonverbal Pain Scale (NVPS) Tool for pain assessment
Assessing pain in patients with cognitive impairment in acute care
Pain Assessment in Advanced Dementia Scale (PAINAD)
Pain Assessment in Non-Communicative Adult Palliative Care Patients
Pain Assessment in People with Dementia
Tools for Assessment of Pain in Nonverbal Older Adults with Dementia: A State-of-the-Science Review
Understanding the physiological effects of unrelieved pain
Untreated Pain, Narcotics Regulation, and Global Health Ideologies
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death