-

A Complete Guide to Hiring Caregivers for Terminally Ill Patients
Discover the essentials of hiring caregivers for terminally ill patients. This guide covers caregiver qualifications, assessing understanding of terminal care, and practical hiring tips. -
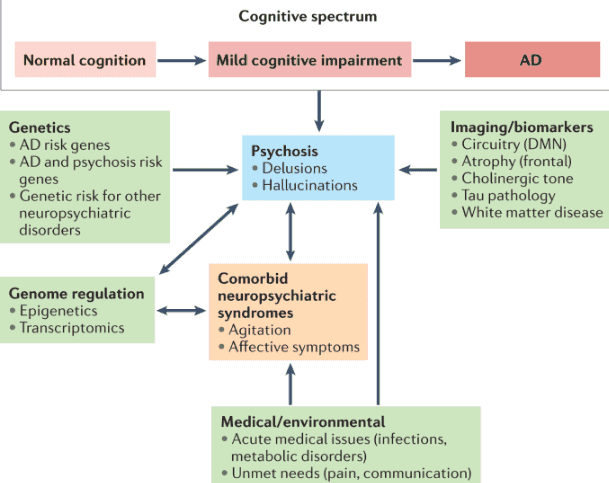
A Comprehensive Guide to Dementia-Induced Psychosis for Hospice Care Providers
This guide provides hospice nurses, caregivers, and family members with essential information on dementia-induced psychosis, including its signs, symptoms, differentiation from other conditions, and effective management strategies. -

A Comprehensive Guide to Diabetes Management for Loved Ones with Dementia
Discover essential strategies for managing diabetes in loved ones with dementia. This comprehensive guide covers blood sugar monitoring, medication administration, diet management, and recognizing emergencies, empowering caregivers to provide optimal care. -

A Comprehensive Guide to Diagnosing Dementia and Providing Compassionate Care
Dementia is a complex condition affecting millions worldwide. Diagnosing dementia requires the expertise of medical professionals specializing in cognitive disorders. By guiding families and caregivers through the diagnostic process, you can empower them. In this article, we’ll explore the steps to find the right specialist for a dementia diagnosis and how families can prepare for the crucial doctor visit. -

Abdominal Aortic Aneurysm: A Life-Threatening Condition for Hospice Patients
The purpose of this article is to provide you with some information and guidance about AAAs and how they can be managed in hospice patients. -

Adrenal Insufficiency Crisis Management for Terminally Ill Patients
Discover essential strategies for managing adrenal insufficiency crises in terminally ill patients. Learn about symptoms, risk factors, and crucial interventions to ensure patient comfort and safety. This guide provides valuable insights for hospice nurses and caregivers in this critical condition. -

Advocating for Your Terminally Ill Loved One in a Facility
As a family member of a terminally ill loved one receiving care in a facility, you play a vital role in ensuring they receive the best possible care and support during their journey towards a good death. Advocating for your loved one involves understanding their needs, communicating effectively with the facility staff, and staying informed about their care plan. This article aims to guide you on being an effective advocate, asking the right questions, and ensuring your loved one’s comfort and well-being. -
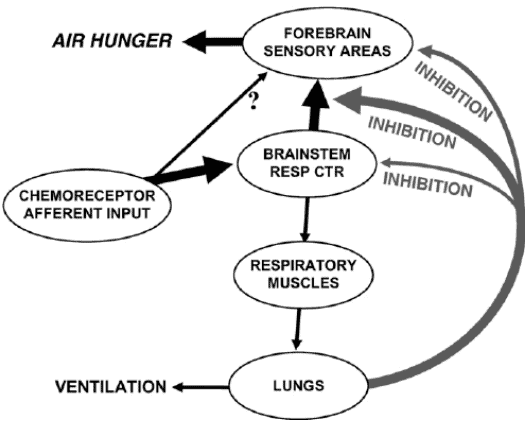
Air hunger management at end-of-life
I can count the times I’ve run into air hunger at the end of life as a visiting RN Case Manager for going on five years on one hand. Over the years, I’ve managed patients with pulmonary fibrosis, lung cancers (diverse types), breast cancer, COPD, congestive heart failure, B-cell lymphoma, leukemia, and other diseases that can impact one person’s ability to breathe correctly. Air hunger is rare in my firsthand experiences, but it can happen. Air hunger often sounds like the person is gasping for breath without regard to the actual respiratory rate (how fast they are breathing); it can also sound like stridor (YouTube videos below where you can hear the difference). -

Aromatherapy for Life’s Challenges: Supporting Anxiety, Grief, Loss, and End-of-Life Care
Explore how aromatherapy and essential oils relieve anxiety, grief, loss, and critical symptoms like pain and nausea across all stages of life. Practical, safe use tips are provided for caregivers, doulas, and health professionals to support holistic well-being. -
Assessing pain in non-verbal patients
Pain is a subjective sensation that can affect a person’s physical, emotional, and spiritual well-being. While pain can be measured objectively by using vital signs such as temperature, pulse, blood pressure, and respiration count, these indicators may not reflect the true intensity of pain that a person is experiencing. This is especially true for non-verbal patients, who cannot communicate their pain verbally. Non-verbal patients may include those with advanced dementia, terminal illness, or other conditions that impair their speech. In this article, I will discuss the importance of assessing pain in non-verbal patients, the tools and methods that can be used to do so, and the benefits of providing adequate pain relief for these patients. -

Best Practices for Approaching Combative Dementia Patients
Dementia is a progressive brain disorder that affects a person’s cognitive abilities, memory, and behavior. In the later stages of the disease, some patients can become combative and aggressive, making it difficult for caregivers to provide the necessary care. As a hospice nurse, it’s important to know how to approach and manage combative dementia patients to ensure their comfort and safety. Here are some best practices to consider: -
Best Practices for Oral Care in Hospice Patients: A Guide for Families
Caring for a comatose loved one during their hospice journey requires special attention, particularly when it comes to oral care. In this guide, we’ll explore best practices for oral care, considering the unique needs of comatose patients, and provide you with valuable resources for further guidance. -

Bowel Management for the Terminally Ill: A Guide for Caregivers and Hospice Nurses
Managing bowel problems in terminally ill patients is crucial for their comfort and dignity. This guide offers practical tips for caregivers and hospice nurses to address constipation, diarrhea, bowel obstruction, and ascites, ensuring patients’ better quality of life. -

Bringing Joy and Engagement: How Geri-Gadgets® Transform Care for People with Dementia and Beyond
Geri-Gadgets® are safe, sensory-rich fidget tools designed to help people with dementia, neurodiverse individuals, and anyone who benefits from fidgeting. These colorful, non-toxic products improve mood, reduce anxiety, encourage engagement, and support physical and cognitive health. Learn how these innovative tools can transform care. -
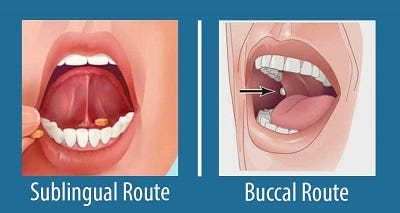
Buccal vs Sublingual for Liquid Medications
Your dying patient has lost their gag reflex as part of the dying process. One of the questions I implore you to ask yourself is what’s the safest route to administer liquid medications? Well, before even going to answer this question, unless contraindicated, make sure the patient’s head of the bed is at least at a 30 to 45-degree angle (I prefer the latter). The buccal route is the safest route to administer liquid medications at the end of life in my experience. In practice, I strongly encourage you as well as the families we mutually teach to give any liquid medications on the side of the mouth least likely to have spillage — this depends on the position of the patient — and slowly over time giving the medication in 0.25 ml increments allowing for the absorption of the medication switching cheeks as applicable.