When There’s No Plan, Families Suffer
Your dad collapses at home. The ambulance rushes him to the emergency room, sirens blaring, paramedics already starting chest compressions before they even reach the hospital doors. His heart stops. The ER team starts CPR, breaking ribs in the process, blood pressure dropping, monitors beeping frantically, while nurses scramble to insert IV lines.
They put him on a ventilator. He never wakes up.
For six weeks, your family argues about what he would have wanted. Your brother insists Dad would fight to stay alive. Your sister remembers him saying he’d never want machines breathing for him. The arguments turn vicious. Relationships crack under the weight of impossible decisions made in hospital hallways at 3 AM.
No one really knows what Dad wanted.
This happens every single day in hospitals across the country.
The Hospital System Isn’t Built for Dignity
Emergency room staff are trained to do one thing: save lives at all costs. They don’t know your dad hated the idea of machines keeping him alive. They don’t know he told you last Christmas he’d rather die peacefully than suffer in a hospital, that he watched his own father waste away in an ICU and swore he’d never put his family through the same nightmare.
They can’t consider his dignity, his values, or his definition of quality life because their job is to rescue and maintain life. Period. Comfort doesn’t factor into emergency protocols. Respect for your wishes takes a backseat to the legal requirement to intervene. They will break bones, insert tubes, and attempt to shock hearts back into rhythm regardless of age or circumstances.
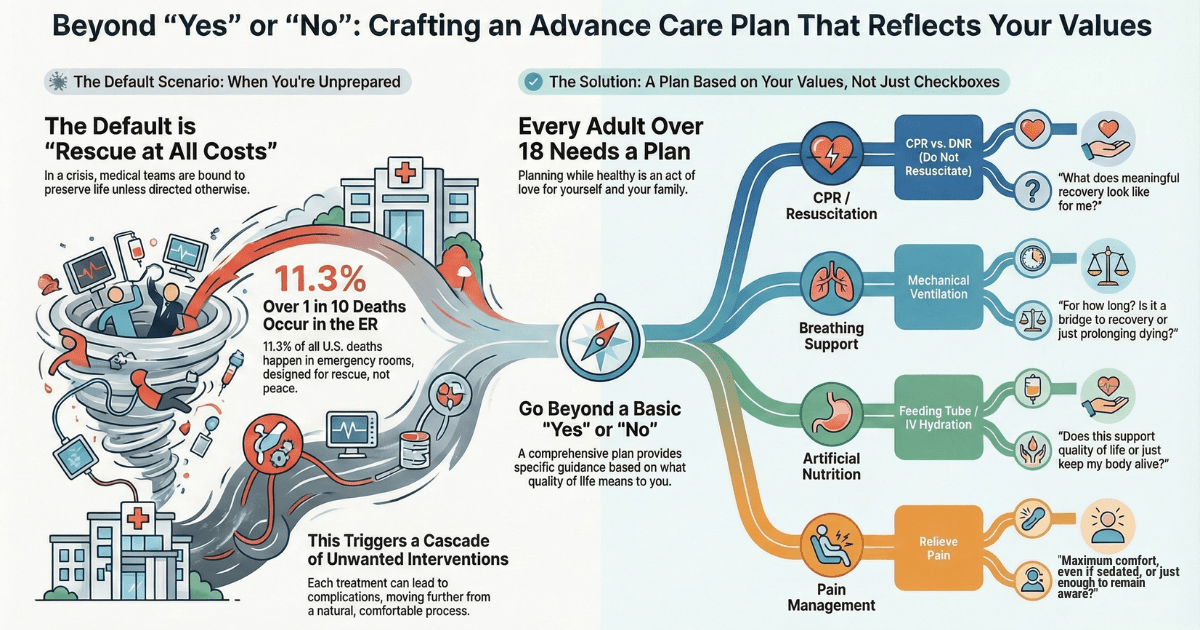
Here’s what they won’t tell you: At best, only 20% of people who receive CPR in the hospital survive the initial event.
That means 80% die anyway despite the broken ribs and traumatic intervention. But even for that 20% who survive? Of those survivors, 80% end up in the ICU for two weeks, and of those ICU patients, 80% are left with lifelong disabilities. Brain damage. Chronic pain. Loss of independence. The ability to eat, walk, or recognize their own children stolen by the very intervention meant to save them.
Yet without clear advance directives, doctors must perform CPR. It’s the law. Your suffering becomes a legal obligation.
Four Devastating Consequences of Avoiding This Conversation
1. Your family makes agonizing decisions during the worst moments of their lives
When emotions are running high and clear thinking is nearly impossible, your loved ones will be forced to guess what you would want. They’ll replay every conversation, searching for clues. They’ll wonder if that offhand comment five years ago was really your final wish or just something you said while watching a sad movie.
2. Siblings stop speaking to each other
Family conflict over medical decisions permanently destroys relationships. Your daughter, who chose to remove life support, will carry guilt forever, wondering if she gave up too soon. Your son, who wanted to keep fighting, will resent her for the rest of his life. Holiday dinners become silent battlegrounds. Grandchildren grow up barely knowing their cousins because the adults can’t be in the same room.
3. You receive aggressive treatment you never wanted
Research shows that 37% of people with advanced cancer receive treatment that doesn’t match their personal goals. That’s more than 1 in 3 people suffering through care they never wanted, simply because they didn’t plan ahead. Ventilators. Feeding tubes. Dialysis that keeps you alive but removes every shred of dignity you hoped to maintain. Pain that could be managed with proper sedation, but isn’t, because no one knows you’d rather be comfortable than alert.
4. Financial devastation compounds the emotional trauma
Treatments that Medicare may not fully cover, hospital bills that drain savings meant for your grandchildren’s education, and legal fees to establish guardianship because you never designated a financial power of attorney. Your family inherits debt along with grief.
Meet Peter M. Abraham: Your Guide Through This Process
You need someone who’s been at hundreds of bedsides. Someone who knows exactly what happens when things go wrong. Someone who understands medical protocols from the inside and can translate your values into instructions that emergency room staff, ICU doctors, and specialists will actually follow.
Peter M. Abraham, BSN, RN, is an experienced registered nurse specializing in advanced illnesses and a health and life navigation specialist at Compassion Crossing, LLC. His nursing background means he knows what CPR really looks like, how ventilators feel, what “comfort care” actually means in practice, and which questions you need to answer before crisis hits.
Peter doesn’t hand you a generic form and wish you luck. He sits down with you for in-depth conversations about the medical realities most people never hear until it’s too late, then helps you create a complete, value-based set of advance directives that protect both your dignity and your family’s peace of mind.
Value-Based Advance Care Planning: What You’ll Create
This isn’t about filling out paperwork. This is about understanding what matters most to you, then translating those values into crystal-clear medical instructions that leave no room for confusion, no space for family members to argue over interpretation, no chance that a well-meaning doctor will do something you explicitly didn’t want.
The Deep Dive Conversations
Peter will guide you through honest discussions about decisions you didn’t know you could make:
- Cardiopulmonary resuscitation and do-not-resuscitate orders – What really happens during CPR, survival rates and long-term outcomes, what choosing DNR actually means for your care, and how to communicate this to family members who might panic at the phrase “do not resuscitate.”
- Breathing support beyond mechanical ventilation – From oxygen masks to BiPAP machines to full ventilators, understanding each level of intervention and where you draw the line.
- Antibiotics – When treatment helps and when it simply prolongs dying without adding comfort or quality.
- Artificial nutrition and hydration – Feeding tubes, IV fluids, and comfort-focused alternatives that honor your body’s natural process.
- Dialysis – This life-extending treatment requires multiple sessions per week and significantly impacts quality of life; you have the right to refuse it or stop it at any time.
- Pain management and sedation levels – You can actually specify exactly how much sedation you want, from alert enough to talk with family to deeply comfortable and unaware; most people don’t know they can choose this.
- Implanted cardiac defibrillators – If you have an ICD, you can specify whether to turn it off when your condition progresses.
- Additional interventions based on your unique health situation and values.
Your Complete Document Package
When you complete advance care planning with Peter, you’ll have:
- Living Will – Crystal-clear medical treatment preferences that specify exactly which interventions you want and which you refuse.
- Durable Medical Power of Attorney – Choosing the right person to speak for you when you can’t speak for yourself, with guidance on how to prepare them for this responsibility.
- Durable Financial Power of Attorney – Protecting your financial decisions so your family doesn’t need court intervention to pay your bills or manage your accounts.
- POLST/MOST/MOLST Form Guidance – Peter will help you fill out this critical physician order form, making sure everything aligns with your values and nothing contradicts across your documents.
- Optional Addendums for specific situations:
- Dementia care preferences if cognitive decline is a concern.
- Psychiatric advance directives for mental health treatment.
- Voluntarily Stopping Eating and Drinking (VSED) protocols.
- Additional specifications based on your unique needs.
Everything will be written in plain language, so your family and doctors can easily understand. No legal jargon. No medical terminology without explanation. No ambiguity that leaves room for misinterpretation.
Your Next Step: Book a Free Conversation
You don’t have to figure this out alone.
Schedule a free initial conversation with Peter M. Abraham to discuss your situation, ask questions, and learn how advance care planning can protect both you and the people you love.
No pressure. No sales pitch. Just an honest conversation about what matters most and how to make sure your wishes are honored when you need them to be.
Schedule Your Free Conversation Now
During this free conversation, you’ll discover:
- Whether advance care planning is right for you (and why the answer is almost always yes).
- What the process looks like from start to finish.
- How long it takes to complete your documents.
- What questions should you start thinking about before your first full session.
Don’t Wait Until Crisis Forces Your Hand
Your family shouldn’t have to guess. They shouldn’t stand in hospital hallways at 2 a.m. trying to remember whether you said you’d want a feeding tube or were just asking hypothetical questions. They shouldn’t break relationships over medical decisions you could have clarified in a few conversations.
Hospital staff will follow protocols regardless of what you would have wanted, because their legal obligation is to rescue and maintain life, not to honor preferences you never documented. Crisis doesn’t wait for convenient timing. It doesn’t care that you were planning to have this conversation next month. It doesn’t give you a warning before it arrives.
Take the first step today. Your future self will thank you. So will your family when they can focus on loving you instead of arguing about you.