-

Top 30 FAQs About Hospice: Everything You Need to Know
Discover hospice care, eligibility, benefits, provider choice, costs, services, and more. Learn how hospice addresses physical, emotional, spiritual, and social needs and how to prepare for and manage them. Find out about the roles of the hospice team and the primary caregiver and the signs of approaching death. Empower yourself with the knowledge to make informed decisions about compassionate end-of-life care. -

Identifying Patients Who May Benefit from Hospice Care: A Visual Observation Guide for Personal Care Facilities
Identifying when a patient may benefit from hospice care is a critical yet often challenging task. For caregivers, including Certified Nursing Assistants (CNAs) and Medical Technicians (Med Techs), visual observation can be a powerful tool for recognizing signs that suggest a hospice referral might be appropriate. This guide is tailored to assist caregivers in personal care facilities in identifying these signs through visual observation methods, helping provide compassionate and timely end-of-life care.
-

A Day In The Life Of A Hospice Nurse
What does a typical day, a typical week look like for a visiting hospice registered nurse case manager look like? -
A Holistic Approach: Hospice Nursing Assessment vs. Hospital/Nursing Home Assessment
Explore the compassionate approach of hospice nursing assessments, emphasizing patient comfort and dignity over conventional hospital metrics. This article delves into the personalized care that defines hospice evaluations, ensuring a serene transition for patients and families. -
Caring for Your Terminally Ill Loved One: Home or Facility Care?
Deciding between home care and facility care for a terminally ill loved one requires careful consideration of medical, emotional, and practical factors to ensure comfort and dignity. -

Caring in Crisis: Navigating the Challenges of Hospice Care in 2023
Hospice care is a vital form of healthcare dedicated to providing comfort and support to patients in their final stages of life. While it’s a relatively recent concept in the United States, with its inception in 1974, it has gained significant popularity, with over half of Medicare beneficiaries in 2020 receiving hospice services. Nevertheless, as we delve into 2023, hospice care confronts several formidable challenges. These include labor shortages, concerns about the quality of care, and the notable presence of for-profit entities in the industry. In this article, we will navigate through the history of hospice care in the United States, its present state in 2023, and the challenges that affect not only hospice patients but also the dedicated staff and providers. -
Celebrating the Legacy of Florence Nightingale in Hospice Nursing
In the realm of nursing, the spirit of Florence Nightingale, the pioneer of modern nursing, continues to illuminate the path for nurses across various specialties. Her legacy, rooted in compassion, patient-centered care, and unwavering dedication, resonates deeply with nurses from all walks of life. However, we discover a profound connection to Florence Nightingale’s nursing model within hospice nursing. This article will explore the distinctive qualities that set hospice nurses apart, including their remarkable autonomy, acute assessment skills, problem-solving abilities, and holistic approach to patient care. -

Choosing Compassion: The Case for Hospice Care
When a loved one is facing a serious illness, it can feel like standing at a crossroads. Each path represents a different way to care for them in their time of need. It’s a moment filled with tough choices and deep emotions. This article thoroughly explains hospice care, its philosophy, and the benefits it provides to patients and families facing terminal illness. Learn about the decision-making process, the hospice experience, and how to navigate this difficult choice with dignity and love. -

Choosing Your Hospice Care: Understanding Patient and Family Rights
An article that guides families through understanding and exercising their rights to choose the best hospice care for their loved ones, ensuring their final chapter is written with compassion and respect. -
Common Medical Abbreviations and Terminology in Hospice
Discover the language of compassionate end-of-life care with this guide to common medical abbreviations and terminology in hospice. From team member roles to levels of care and clinical terms, this article provides valuable insights for patients, families, and caregivers navigating the hospice journey. -

Compassionate Care at Home: How Hospice Supports Families and Their Terminally Ill Loved Ones
In-home hospice care offers a sanctuary of comfort and support for terminally ill loved ones and their families. It brings medical care, emotional solace, and practical help to your doorstep, allowing patients to spend their final days in the warmth of home. Learn how hospice care can provide personalized support, ensuring dignity and quality of life. -

Comprehensive Guide to Financial Assistance for Hospice and Palliative Care Patients
Learn about various financial assistance options available for terminally ill patients who need hospice or palliative care but lack Medicare, Medicaid, private insurance, or the means to self-pay. -
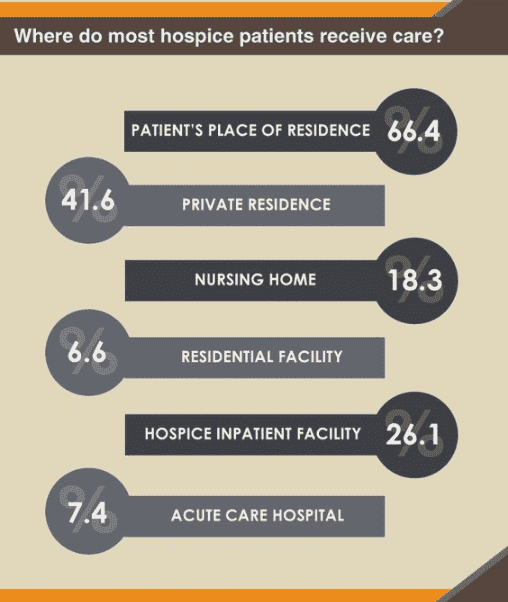
Considering Home Hospice vs. Hospice at a Facility: Making an Informed Decision
Deciding on end-of-life care for a loved one is challenging and emotional. One major decision to make is whether to opt for home hospice or hospice care at a facility. Both options have advantages and drawbacks, and understanding the pros and cons can help families make an informed choice. Here, we’ll explore the pros and cons of each option and provide key questions that families should ask themselves to aid in their decision-making process. -

Demystifying Death: Why Hiding the Dying Process from Children Harms Society’s Future
Shielding children from death deprives them of understanding this natural part of life, leading to emotional and psychological consequences. This article explores why exposing children to the dying process is essential for their development and highlights the role of hospice care in supporting families during this time. -

Dispelling Myths About Hospice Care
Hospice care is often misunderstood and shrouded in myths that can prevent individuals and families from accessing the compassionate support they need during a challenging time. This article will address common misconceptions about hospice care and provide you with the facts. We aim to empower you with accurate information to make informed decisions when considering hospice for yourself or a loved one. -
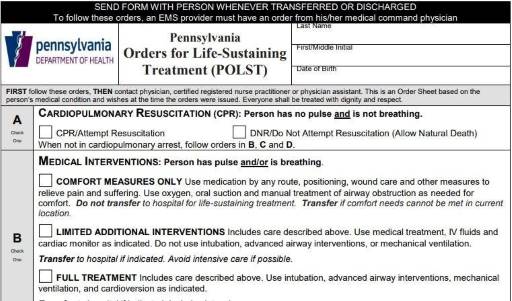
DNR and the Terminally Ill
Navigating conversations about Do Not Resuscitate (DNR) orders with terminally ill patients and their families can be challenging yet crucial for ensuring that the patient’s wishes and comfort are prioritized. The decision between opting for DNR or full code often involves delicate emotions, medical considerations, and ethical concerns. In this article, we will delve into a methodology that has proven effective in facilitating these discussions, particularly in the context of hospice care. Drawing from years of experience and successful outcomes, we’ll explore approaches that prioritize compassion, clarity, and patient-centered care. Additionally, we’ll reference valuable resources to enhance understanding and guide these critical conversations. -

Do You Need Hospital Experience to Be a Hospice Nurse?
In this article, we will explore whether medical-surgical or critical care experience is necessary to become a hospice nurse, the benefits and challenges of working in hospice care, the educational and licensure requirements for hospice nurses, and the resources and opportunities for professional development and networking in hospice nursing. -

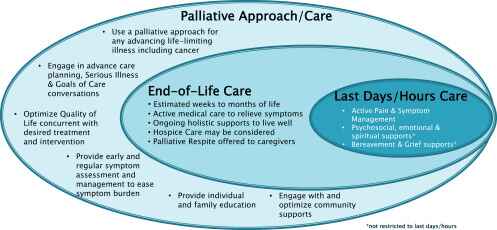
Embracing the Journey: Understanding the Transition to Hospice Care
This detailed guide provides insights into the transition from palliative care to hospice, offering practical advice and emotional support to patients, caregivers, and family members during this critical phase. -

End-of-Life Decisions: Don’t wait until it’s too late for advanced directives
Autonomy, the right to receive or refuse medical treatment is a crucial element of health care ethics (American Nurses Association (ANA), 2011; Plakovic, 2016). Nurses are involved in helping patients and families be aware of when end-of-life is occurring, and in educating the patient and family about end-of-life legislation that helps guide everyone committed to continue the right of patient autonomy when the patient is no longer able to express their wishes. Before the Patient Self Determination Act, we had the famous cases of Karen Ann Quinlan and Nancy Cruzan who were, from a point-of-view, forced to suffer for ten or more years of futile treatment (Miller, 2017). Now, we have advanced directives that allow patients to express their wishes while they are able, yet we still have ethical dilemmas when either those needs are expressed vaguely or not at all. It is in the best interest of the patient and the patient’s loved ones for advanced directives to be utilized and kept up to date. -

General Inpatient (GIP) Level of Care for Hospice Explained
GIP, or General Inpatient Hospice, is an often misunderstood aspect of hospice care. Both hospital staff and families sometimes have misconceptions about GIP. Families may assume it’s readily available upon request, while hospital professionals may believe it allows patients to remain in the hospital indefinitely, even when death is weeks away. This article will clarify the basics of GIP for hospice, including eligibility requirements, doctor’s orders, care plans, documentation, and education. We’ll conclude with two real-life cases to illustrate these points.