
Should dying patients be on oxygen?
I have cared for many terminally ill patients over the years. One question that comes up frequently is should the dying patient be on oxygen at the end of life?
I see it from both sides, from hospice intake personnel as well as the admitting nurse — all had it drilled into them over the years that low oxygen saturation must be treated — to families who see how hospital and nursing home staff rush to put someone on oxygen because of low oxygen saturation.
Contrary to widespread belief, most dying patients do not need oxygen. Here’s why:

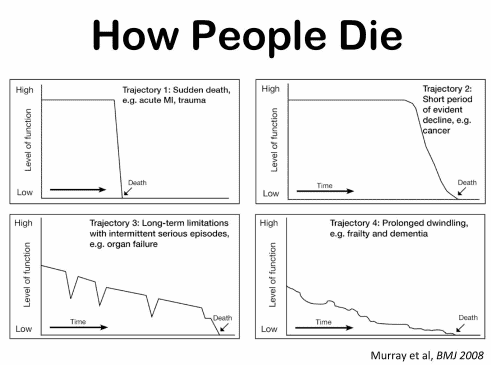
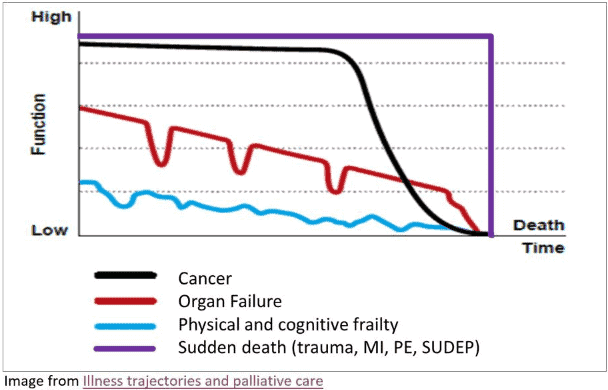
Frequency of Changes in Condition as an Indicator of Approaching Death
Recognizing the velocity of changes in a patient’s condition is crucial for hospice nurses. By understanding the pace of changes in vital signs, symptoms, functionality, and more, nurses can anticipate needs, adjust care plans, and communicate the prognosis effectively with patients and families. The article provides guidelines on interpreting the velocity to estimate the time a patient has left.

Best Practices for Approaching Combative Dementia Patients
Dementia is a progressive brain disorder that affects a person’s cognitive abilities, memory, and behavior. In the later stages of the disease, some patients can become combative and aggressive, making it difficult for caregivers to provide the necessary care. As a hospice nurse, it’s important to know how to approach and manage combative dementia patients to ensure their comfort and safety. Here are some best practices to consider:

Recognizing and Treating Common End of Life Symptoms
Guide to Recognize and Treat Common End of Life Symptoms provides tips on managing symptoms experienced by those at the end of their lives – Topics such as pain, shortness of breath, respiratory distress, and anxiety, and provides suggestions for medications and complementary therapies to help manage these symptoms.

The Dark Side of Physical Therapy for Geriatric Patients with Dementia
Explore the ethical dilemma of physical therapy for terminally ill dementia patients. This article examines the potential harm of aggressive interventions, highlighting the importance of comfort-focused care. Learn why hospice professionals often advocate for gentler approaches in end-of-life dementia care.

Terminal Restlessness in the Completely Nonverbal Patient
Terminal restlessness is a common phenomenon that occurs in the final stages of life. It is characterized by agitation, confusion, and distress. It can be challenging to recognize and manage, especially in patients who cannot communicate verbally. This article aims to share insights and tips from a hospice worker who learned how terminal restlessness can manifest differently in nonverbal patients and how to cope.
End-of-Life Determinations for Newly Admitted Patients
Admitting a patient to hospice services is a complex and sensitive process that requires careful assessment and communication. One of the challenges that hospice nurses face is to determine if the patient is close to the transitioning phase of dying, which is the final stage of life when death is imminent. This phase usually lasts for one to two weeks, and it is essential to prepare the family and provide a plan for increased hospice involvement during this time. However, on admission, hospice nurses do not have the luxury of having visited with the patient over the past several weeks to months to observe the changes that often signal that death is approaching. Therefore, they need to rely on other indicators to help them identify whether the patient is transitioning.
Educating families on reporting changes in condition
When someone you love is sick and may not get better, you want to do everything possible to make them comfortable and happy. Sometimes, you may notice that they are acting differently or feeling worse. This is called a change of condition. Some changes in condition are very serious and need to be reported to the hospice provider right away. Other changes in condition are less urgent and can be written down in a journal until the next nursing visit. This article will help you learn how to tell the difference and what to do.
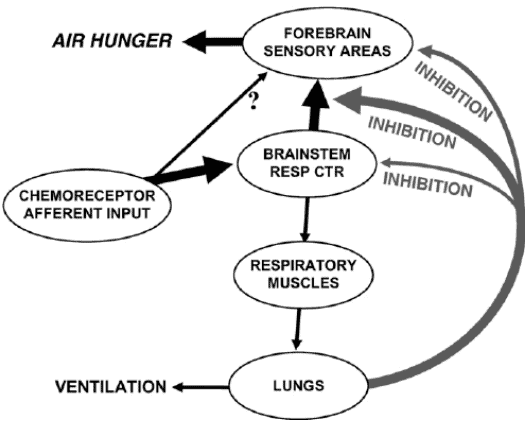
Air hunger management at end-of-life
I can count the times I’ve run into air hunger at the end of life as a visiting RN Case Manager for going on five years on one hand. Over the years, I’ve managed patients with pulmonary fibrosis, lung cancers (diverse types), breast cancer, COPD, congestive heart failure, B-cell lymphoma, leukemia, and other diseases that can impact one person’s ability to breathe correctly. Air hunger is rare in my firsthand experiences, but it can happen.
Air hunger often sounds like the person is gasping for breath without regard to the actual respiratory rate (how fast they are breathing); it can also sound like stridor (YouTube videos below where you can hear the difference).
Understanding Changes in Diet Texture for the Terminally Ill
Navigating the dietary needs at life’s end can be complex. This guide explores the progression of diet textures and liquid consistencies, ensuring comfort and safety for the terminally ill. Learn to adapt meals for loved ones as they approach this delicate phase.

Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Naomi Feil is an expert in gerontology and the creator of validation therapy, which is a means of communicating and acknowledging the internal reality of patients with dementia. When properly utilized, validation therapy can enhance the quality of life of patients with dementia as well as reduce stress on the family and caregivers.
While Naomi Feil and her followers (of which the writer of this article may be considered one, at least in form) focus on using this method of communication to maintain health with the potential for a level of restorative health, I want to share how the concepts of this method can be used during times of crisis.

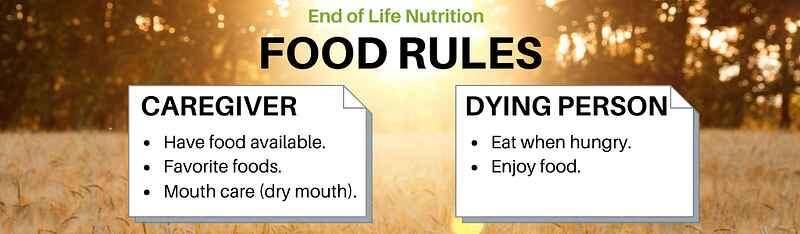
Food and Liquids During the Dying Process
This article explores the delicate balance of providing food and liquids to the dying and navigating the complexities of end-of-life care. It addresses the emotional and ethical considerations, offering guidance for caregivers during this profound phase.
