
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Naomi Feil is an expert in gerontology and the creator of validation therapy, which is a means of communicating and acknowledging the internal reality of patients with dementia. When properly utilized, validation therapy can enhance the quality of life of patients with dementia as well as reduce stress on the family and caregivers.
While Naomi Feil and her followers (of which the writer of this article may be considered one, at least in form) focus on using this method of communication to maintain health with the potential for a level of restorative health, I want to share how the concepts of this method can be used during times of crisis.

Fall Reduction – Reducing Falls in Personal Care Homes and Private Homes
Falls among the elderly can have severe consequences, including hip fractures, which can be life-threatening. As an experienced hospice registered nurse case manager, I understand the importance of fall prevention, especially in private homes, personal care homes, and assisted living facilities. This article aims to provide practical tips for reducing falls in these settings by following the nursing process: assessment, diagnosis, planning, implementation, and evaluation.
Assessing pain in non-verbal patients
Pain is a subjective sensation that can affect a person’s physical, emotional, and spiritual well-being. While pain can be measured objectively by using vital signs such as temperature, pulse, blood pressure, and respiration count, these indicators may not reflect the true intensity of pain that a person is experiencing. This is especially true for non-verbal patients, who cannot communicate their pain verbally. Non-verbal patients may include those with advanced dementia, terminal illness, or other conditions that impair their speech. In this article, I will discuss the importance of assessing pain in non-verbal patients, the tools and methods that can be used to do so, and the benefits of providing adequate pain relief for these patients.
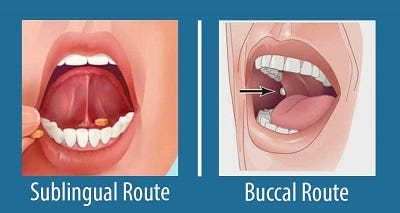
Buccal vs Sublingual for Liquid Medications
Your dying patient has lost their gag reflex as part of the dying process. One of the questions I implore you to ask yourself is what’s the safest route to administer liquid medications? Well, before even going to answer this question, unless contraindicated, make sure the patient’s head of the bed is at least at a 30 to 45-degree angle (I prefer the latter).
The buccal route is the safest route to administer liquid medications at the end of life in my experience. In practice, I strongly encourage you as well as the families we mutually teach to give any liquid medications on the side of the mouth least likely to have spillage — this depends on the position of the patient — and slowly over time giving the medication in 0.25 ml increments allowing for the absorption of the medication switching cheeks as applicable.

Understanding Terminal Restlessness
Navigating the final days of a loved one’s life can be a challenging and emotional journey. One of the signs that can be observed during this time is known as terminal restlessness. As someone deeply rooted in hospice care, I have witnessed various manifestations of this restlessness. Understanding its types, causes, and management strategies is crucial for providing compassionate end-of-life care. This article aims to illuminate the different kinds of terminal restlessness, identify reversible causes, and discuss effective management techniques. By equipping caregivers, families, and healthcare professionals with this knowledge, we can ensure that terminally ill individuals experience comfort and dignity in their final days.
